Unfinished Business, Pt 3
Media acknowledgement of the Paxlovid viral "rebound," and more evidence supporting the Official Unglossed Theory of why the rebound is occurring.
Continued from “Unfinished Business.”
Researchers in Boston announce both experiencing and launching studies into the Paxlovid rebound phenomenon; and the early report of a case study involving sequencing accords with the Official Unglossed Totally Reckless Theory of the mechanism behind it.
Nothing But Net
The Official Unglossed Totally Reckless Theory™ (OUTRT) for how Paxlovid could be creating a temporary pause, and then resurgence (“rebound”) of viral replication and symptoms in some number of recipients… really may not have been so reckless after all.
Besides the anecdotes unearthed beforehand by Igor Chudov, and the FDA Emergency Use Authorization review which turned out to feature tangible evidence that accords with my “Paxlovid Viral Rebound” theory, a Boston Globe story piles on more corroboration. This post is simply a brief review of those new developments.
As before, all credit for the discovery of this possible medical fiasco continues to go to Chudov. Here is his original post; and see Part 1 of my series for description of the theory; and see Part 2 for my appraisal of the evidence in the FDA review.
(Not) “Puzzling”
As mentioned in Pt. 1, what struck me when originally reading the anecdotes about Paxlovid rebounds is that the mechanism to explain the rebound is so obvious, I should have thought of it beforehand, at least had I devoted any time to researching or thinking about Pfizer’s drug.
So, it’s amusing that now that the phenomenon is breaking in the wider expert consciousness, it is being referred to as somehow “puzzling.”1

A granular quotation of the Globe’s report, hyperlinks included, is the most efficient way to cover the relevant points of corroboration it offers with Parts 1 and 2:
But now some patients are reporting on social media an unusual and unnerving phenomenon: their COVID symptoms appear to rebound after taking the medication.
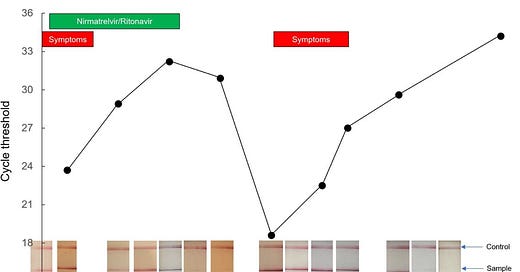
And it’s not just their symptoms that reappear. Many report that after finishing their five-day course of treatment, feeling better, and testing negative on an at-home rapid test, they then test positive again a few days later. [All of this recapitulating the reporting already provided by Igor Chudov.] […]
John Donoghue, a 71-year-old emeritus physics professor in Amherst[…], his wife, and her 95-year-old mother all were infected with COVID in the last month. All three received Paxlovid, felt better, and tested negative on rapid tests for four or five days. Then their symptoms returned and each one tested positive again. […]
But some infectious disease specialists, while still extolling Paxlovid’s benefits, have expressed concern that the rebounds they are seeing and hearing about may indicate patients, after completing treatment — and testing negative and then positive, again — may still be infectious and transmitting the virus to others.
Dr. Kathryn Stephenson, an assistant professor at Harvard Medical School and an infectious disease physician at Beth Israel Deaconess Medical Center[…] is researching why some people in a household get infected with COVID while others do not. She is enrolling volunteers in the study and said she expects to also examine why some patients who’ve taken Paxlovid get sick again.
And so, the consensus now seems to consider the anecdotes originally discovered by Chudov as part of a bonafide trend, at least in the Boston area where a critical mass of experts seem to have encountered the phenomenon first hand!
Now to the portions of the report that detail the current state of investigation into the rebound:
The issue has captured the attention of at least two teams of Boston-area scientists, who are trying to understand what might be fueling the problem. Resistance to the drug? [Not quite.] Patients being quickly reinfected? [No.] Or maybe some people just need to take the medicine longer to mount a more effective immune response. [Not quite.]
Both of the first two listed possible mechanisms, resistance and reinfection, seem to fail to find confirmation a case study. Note that “resistance,” in the sense normally applied to bacterial infection, would imply that the sequence of a post-rebound sample of the virus shows some sort of resistance-conferring mutation, particularly in the genes for the nsp5 (or “Mpro,” or “3C-Like”) Polyprotein-Chopping Protein targeted by the drug. “Reinfection” would imply that the sequence of a post-rebound sample appears to be “unrelated” to the original infection.
An intrinsic rebound mechanism - as proposed by my theory that the virus simply “picks up where it left off” when still-unchopped polyproteins in already-infected cells release more nsp5 - wouldn’t necessarily show any difference in the post-rebound sequence.
But in a way, this is “resistance” - only, the virus isn’t evolving to gain the trait that gives it resistance, it is already built into its default replication cycle.
Mutation is not needed for Paxlovid resistance
Anti-Paxlovid SARS-Cov-2 “mutant” trait = nsp5 auto-cleavage (Paxlovid arrests Orf1 breakdown before nsp5 has self-cleaved, by slowing self-cleavage, but not actually stopping it) + increase in nsp5 cleavage efficiency after each discrete self-cleavage, reversing the arrest = Normal SARS-CoV-2 design
Thus, when the Globe reports:
Pfizer noted [actually, the FDA reviewers noted, but good try, Boston Globe] in the documents submitted last fall to federal regulators for its emergency use authorization that “several subjects appeared to have a rebound in SARS-CoV-2 RNA levels around Day 10 or Day 14” but said that “currently there are no clear signals” the virus had developed a resistance to one of Paxlovid’s primary components. The documents said Pfizer would continue analyzing the data.
What is really being described is that the rebound was observed regardless of any mutations to the nsp5 genes, just as described in Part 2 of my series. It is not a product of evolution prompted by Paxlovid; it is just something the virus can already do.

Further, the Globe reports:
Dr. Michael Charness, chief of staff at the VA Boston Healthcare System, recently completed an in-depth study of one patient who experienced a rebound after taking Paxlovid. [Edit, April 28: The Charness case study is now available in preprint, see footnotes.2]
Charness sequenced three nasal swabs from the patient and tested the patient for a battery of other respiratory illnesses. He concluded that the virus was not resistant to Paxlovid [in the sense of mutating to acquire a novel resistance, as with antibiotic-“resistant” bacteria] and that the patient had not been infected with any other respiratory viruses or other variants of COVID. Rather, he concluded some patients may need a longer course of treatment for their immune system to mount a robust defense.
“Experienced a rebound” links to the summary of the case study provided by Charness in a reply to another online discussion of the trend:
“Sequence same at 3 time points.”
As if the virus that is replicating post-rebound is exactly the same as the one that Paxlovid “paused” inside of already-infected cells. Why, what could cause that?
Overtime?
One point I would like to add, though I will possibly be delving further into it in a yet-to-arrive follow-up on the Paxlovid trial, is why it is “safe” for my theory to assume that already-infected cells contain still-unopened copies of polyprotein (which contain “future” versions of yet-uncleaved, not-Paxlovid-bound nsp5 that will become more efficient at cleavage when eventually auto-cleaved).
I described the logic for this assumption, and how it relates to the question of whether already-infected cells should or shouldn’t be destroyed by the immune system before infection “unpauses,” in a reply to “Bartram,” who writes at Bartram’s Folly and elsewhere, in the comment thread at Chudov’s original post:
[Bartram] Could there be an interaction with vaccine immunity? Ordinarily the antiviral will slow down replication, but there'll still be proteins on the membrane signalling to the immune system to destroy the infected cell -- the antiviral will allow the immune system to control an infection that might otherwise escalate. However, if the vaccines introduce an immune tolerance to the virus then you'll get the observed results -- the infection is controlled by the anti-viral but infected cells aren't cleared and the infection can continue once the anti-virals are stopped.
[Me] Above, I speculated "Covid vaccines suppressing the innate immune system," but tolerance could be playing a roll. It depends on whether spike is already being MHC-presented, and/or whether it is dominant, when the nsp5-block takes effect. To a certain extent it's axiomatic that the block / pause occurs when the virus still needs more Orf1 polyproteins to be cleaved (otherwise the drug wouldn't affect replication at all), which is why it's safe for me to assume there are still un-cleaved "future" nsp5's [is it also axiomatic that the pause occurs before nsp5 has self-cleaved? it would at least take perfect timing to pause only just when nsp5 has self-cleaved but before it has broken down the rest of the polyprotein, since this moment is akin to combustion]. This "needs more cleaved Orf1" moment may occur before there is much/any subgenomic mRNA translation in which case, nearby immune cells won't see spike, but just bits of Orf1 nsp's.
For this reason, I would not predict that merely extending the course of Paxlovid beyond 5 days would solve the problem. I am especially pessimistic that “restarting” the course after a return of symptoms3 can do anything but repeat the first experience, though maybe only in a certain percentage of cases. In fact, it may be just as well to shorten the course, to capture the benefit (against severe outcomes) of the “pause” but allow for a quicker arrival at post-rebound recovery.
More in “Unfinished Business”:
Introduction: Early anecdotes
Official Unglossed Totally Reckless Theory Outline
Theory Explanation
Considerations for Covid-vaccine or Omicron interactions
Appraisal of the Paxlovid trial rebound evidence.
Experimental OUTRT confirmation 1: Paxlovid-treated rebound appears to exceed normal PCR test noise, and is not driven by escape mutants.
Part 3 (this post):
Early appraisal of the “Boston Rebound Awakening,” and the Charness case study implications.
Experimental OUTRT confirmation 2: Rebound is not driven by escape mutants or reinfection.
Appraisal of public remarks from Pfizer.
If you derived value from this post, please drop a few coins in your fact-barista’s tip jar.
Lazar, Kay. “A puzzling phenomenon: Patients report a rebound of COVID-19 symptoms after taking the antiviral Paxlovid.” (2022, April 21.) The Boston Globe.
Gupta, K. et al. “Rapid Relapse of Symptomatic SARS-CoV-2 Infection Following Early Suppression with Nirmatrelvir/Ritonavir.” researchsquare.com
No other respiratory viruses were identied at the peak of cold symptoms, and vaccine and developing natural immunity may have minimized symptom severity and duration. Sequencing indicated that this relapse was not due to a treatment-emergent mutation or infection with a different subvariant.
As suggested in the Globe article by Paul Sax, who is also portrayed in the twitter screenshot above.











Brian, I greatly appreciate you digging so deeply into this topic.
Paxlovid was tested on on unvaccinated people only. Now they are giving it to vaxxed people, whose reaction to it, and timeline of development of immune response, is very possibly different from unvaxed.
As your graph shows, paxlovid failed even in some unvaxed people , but seems to be failing much more often (this is just a hunch) in real mostly vaccinated people.
This could be a story not just of Paxlovid failure. This could be a story illustrating vaccine failure of not allowing vaccinated people mount rapid (within 5 days) immune response.
It could also be a story of Omicron not clearing as quickly as Alpha/Delta.
We should keep pushing it.
I tweeted your article from my backup account
https://twitter.com/TotallyCanc3l3d/status/1518046417461424129
Washington Post just published an article about the viral rebound effect with people getting sick from the same infection again (not a reinfection) - https://www.washingtonpost.com/health/2022/04/27/paxlovid-second-case-covid/