Original Antigroundhogic Sin
RE the latest wave of overblown alarmism over breakthrough immune response.
I have previously referred to Original Antigenic Sin as “not real.”1 This is a bit of intentionally provocative hyperbole; what is meant by the hyperbole is that OAS has no coherent meaning in context of actual immune response to actual viruses, and associated outcomes.2
My stand on this subject results in frequent “one-way dialogues” with the substack prophets of Leaky Vaccine Disaster theories. I imagine the regular Unglossed subscriber finds the subject a bit tiring by now. If it helps, try to vicariously relish the satisfaction and pleasure I derive from dismantling the obvious study mis-readings of others. It is like peering at the popular kid’s SAT Reading Test answer sheet to see all the answers they got wrong.3
And as my prior attempts to provide the blogger who goes by “Eugyppius” with free “peer-review” on such mistaken readings were eventually met with (temporary) expulsion,4 I can now write these critiques without the precursory courtesy of pointing out the errors over at his forum.
So, let’s let ‘er rip, full “subtweet” style:

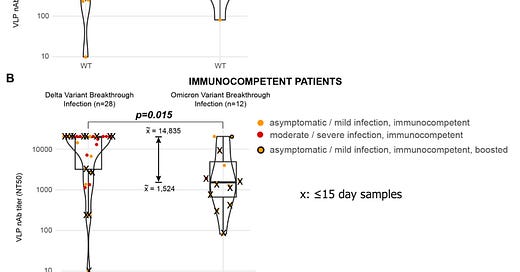
Eugyppius alleges that the study in question demonstrates that OAS is real.5 So, I went and read the study. And indeed, plasma from the Covid-vaccinated patients who were infected with Omicron did not inhibit Omicron as well as the Wild-Type opponent in the virtualized environment of the study’s neutralization assays:
The graphs certainly show that plasma from Omicron-breakthrough patients is better at inhibiting Wild Type and Delta than Omicron.
And, Omicron induces improved neutralization against Wild Type compared to uninfected double-dosed (not pictured above).
Why, it’s as if, it’s as if - The Covid-vaccinated are stuck in Immune Groundhog Day, doomed to churn out the same spike protein antibody design forever, ahhhh! And look - today is literally Groundhog Day!
And yet, my opinion that OAS is Not Real™ remains unchanged. Why?
Because the Omicron patient samples were taken too early for any novel antibodies to be present in the blood.
Thirty-nine of these breakthroughs were probably Delta, and 14 were Omicron.
And 9 of the Omicron breakthrough patients had their blood samples taken less than 15 days after onset of symptoms or positive PCR test. The median number of days post-onset for these nine individuals was 6. The median days to blood sample collection for all Omicron breakthroughs was 8.5:
8.5 days (!) is too early for the arrival of novel, anti-Omicron antibodies. So can testing blood samples from 8.5 days possibly demonstrate whether novel, anti-Omicron antibodies end up being created to begin with? (No!)
While pre-existing memory B Cells against the mRNA-designed spike will obviously ramp up antibodies within a day or two of stimulation - explaining the improvement against Wild Type in the neutralization assay - novel antibodies generated from Omicron infection, by definition, must be developed “from scratch.” It’s an entire process, beginning with Antigen Presenting Cell (primarily Dendritic Cell) migration to the secondary lymphoid organs (primarily lymph nodes). From Akkaya, M. et al.:6
Sure looks like it takes longer than 8.5 days! (It does.)
And even 17 days - the median time for Delta-breakthrough samples - is potentially premature. Novel post-infection antibodies can continue to rise for 30 days after infection with SARS-CoV-2. In the evergreen antibody kinetics paper by Seow, J. et al., the mean time for post-onset seroconversion (arrival of antibodies) against at least one antigen was 12.6 days; and levels of IgG antibody in particular continue rising all the way to day 60 in some patients (while others begin to drop). Their full results, with superimposed markers for 8.5 and 17 days:7
Thus, the evaluation of these early blood samples in neutralization assays against Omicron cannot possibly provide insight into whether novel anti-Omicron antibodies were eventually created. The authors of the study are more-or-less forthright on this point:
Univariate analysis revealed that among the factors examined, only clinical severity, hospitalization for COVID-19, and median numbers of days between symptom onset or PCR positivity and sample collection, were significant.
But does Eugyppius report the same findings to his readers? No. The arbitrary, accidental disparity in sample collection time is subtracted from the statement above, leaving an impression that Omicron’s milder symptoms, alone, account for the only possible “confounding factor” that could create the misimpression of vaccine-induced OAS from these results:
Vaccination plus Omicron gives you about one-third the neutralising activity against wild-type SARS-2, as vaccination plus Delta. As the authors note (p. 16), this is surely down to the mildness of Omicron infection.
Really? Maybe it’s “down” to the later time of sample collection for Delta - with ramped up antibodies no longer having any virus to bind against, levels could be higher on day 17 than day 8.5.
Or, maybe it’s “down” to the lower resemblance between the spike proteins - with memory B Cells for the mRNA-designed spike simply not as well-stimulated by Omicron spike. That wouldn’t be “OAS” - it would be the opposite! The outdated, vaccine-induced memory response is less highly stimulated by the more “novel” version of the spike protein offered by Omicron. Ok, great! Maybe that means the immune system is “taking notice” of the difference!
Note that the authors revive mention of the serum collection timing problem on page 16; though they strangely misrepresent their own attempt to compensate for the problem (emphasis added):
Indeed, we found a significant difference in the median days between symptom onset or PCR positivity and sample collection (Table 1, 17 versus 8.5 days, p=0.008). However, when we analyzed a more comparable subset of samples collected 15 days following PCR positivity and sample collection, the difference in neutralization titers between Omicron and Delta was still significant.
By “collected 15 days,” the authors mean collected 15 days or earlier. But this only recycles the same flaw. If Omicron requires novel antibodies for effective neutralization, and Delta not so much, comparing early-sampled Delta breakthrough plasma performance still doesn’t say anything about performance of novel antibodies; the subject which is at the heart of the OAS hypothesis.
Post-15 days Omicron breakthrough neutralization performance seems improved, if we extrapolate from the authors’ attempted correction. The upper graph represents the authors’ “≤15 days” subset; my edited version of the lower graph, which excludes the ≤15 days dots, reveals that neutralization performance in the 3 immunocompetent “after 15-days” Omicron breakthrough samples is clearly more robust against Wild Type - and comparable to the Delta performance - despite absence of severe infection:
Does this mean that Omicron takes a few more days to stimulate as many vaccine-programed B Cells as Delta? Or maybe that novel Omicron antibodies, once they begin to arrive, have spillover benefit against Wild Type? Who can say - but it certainly supports the conservative suggestion that time of collection for Omicron breakthrough plasma influences neutralization performance.
If there’s an appropriate Groundhog Day reference here, it should be assigned not to the Covid-vaccinated, but to Eugyppius himself, who can’t seem to stop reliving the same episode of misreading the evidence to “confirm” OAS over and over.
In fact, the patently obvious limitations of this study don’t end at sample-time-self-sabotage; and they would be sufficient to dismiss the results even if the samples were less premature.
Firstly, in order to evaluate how these results reflect on the Covid-vaccinated immune response, wouldn’t we also want to ask, “What does the immune response look like for the unvaccinated (either previously infected or not)?” But the authors fail to provide any unvaccinated controls. Firing off conclusions about how the Covid vaccines, specifically, “prime” antibody responses to remain stuck in the mRNA spike design is thus unsupportable.
Secondly, in order to conclude that lower Omicron neutralization implies insufficient anti-Omicron antibody generation, we need to know if “Omicron” (both the Virus-Like-Particle and the cultured virus) is, in fact, equally efficient at infecting the cells in the study’s neutralization simulation as Wild Type and Delta. If it’s more efficient, then the “impaired” Omicron neutralization performance is a reflection, to at least some extent, of that improved tropism for the cells in the assay. Note that the authors used ACE2 + TMPRSS2 expressing cells, implying that Omicron’s dropping of the TMPRSS2 requirement might not confer an advantage.8 But on the other hand, it still might.
Or, the temperature of the neutralization assay could favor Omicron, or on and on. The authors make reference to negative and positive controls in their methods, but as not-plasma-inhibited performance for the three different strains is not reported, there is no way for the readers to evaluate possible flaws in the neutralization assay for themselves. In the end, as the yardsticks for neutralization of Wild Type, Delta, and Omicron might not be equivalent, there is no way to be sure that “lower neutralization” of Omicron in this simulated environment reflects lower antibody response.
Ghosts of OAS Past
Or perhaps the one trapped in Groundhog Day is me. The alarm clock rings, and I’m disputing flimsy “evidence” for OAS again, in an endless loop.
For it just so happens that another flawed nugget of “evidence” that Eugyppius first highlighted in October has been making the rounds again. This is the UKHSA comment on N protein seropositivity among blood donors. My original dismissal of this pseudo-evidence is here:
As I said at the time:
“Recent observations” does not mean observations of recent outcomes. Plenty of “recently” published studies have been time capsules of post-Covid-vaccination infections from the spring [which tend to be asymptomatic or low-symptomatic]. In the review of the “swab” study in September, I lamented that such out-of-date studies could easily be used to unwrite the admission that the Covid-vaccinated can catch and transmit the virus as easily as their unpersoned peers. This has indeed been the case.
Just as easily, such a study could have been used to provide grounds for the comment above, and thus seeded the subsequent declaration that post-“breakthrough” immunity is kaput - in advance of a single shred of evidence that “breakthrough” convalescents are becoming reinfected.
Nothing much has changed. The text in the report today is the same as it was in October, except with an added elaboration that directly supports my interpretation at the time:
[October, 2021] Seropositivity estimates for S antibody in blood donors are likely to be higher than would be expected in the general population and this probably reflects the fact that donors are more likely to be vaccinated. Seropositivity estimates for N antibody will underestimate the proportion of the population previously infected due to (i) blood donors are potentially less likely to be exposed to natural infection than age matched individuals in the general population (ii) waning of the N antibody response over time and (iii) recent observations from UK Health Security Agency (UKHSA) surveillance data that N antibody levels appear to be lower in individuals who acquire infection following 2 doses of vaccination.10
[January, 2022] Seropositivity estimates for S antibody in blood donors are likely to be higher than would be expected in the general population and this probably reflects the fact that donors are more likely to be vaccinated. Seropositivity estimates for N antibody will underestimate the proportion of the population previously infected due to (i) blood donors are potentially less likely to be exposed to natural infection than age matched individuals in the general population (ii) waning of the N antibody response over time and (iii) recent observations from UK Health Security Agency (UKHSA) surveillance data that N antibody levels are lower in individuals who acquire infection following 2 doses of vaccination. These lower N antibody responses in individuals with breakthrough infections (post-vaccination) compared to primary infection likely reflect the shorter and milder infections in these patients. Patients with breakthrough infections do have significant increases in S antibody levels consistent with boosting of their antibody levels.11
And, just as in October, there is no evidence supporting higher rates of reinfection among the Covid-vaccinated. It may be happening; the anecdotes remain prominent; but actual reinfection rates aren’t being measured yet.12 In the mean time, implied alterations of immune response among the Covid-vaccinated are not a surrogate for measurements of actual, real-world outcomes.
If my October-vintage theory that the “recent” observations referred to by the report text were likely focused on early breakthrough infections was valid at the time, then we can suppose either that 1) The text has not been updated to reflect that these studies have ceased to be “recent” 2) Additional observations arrived that rendered the text valid without any updates.
Theory 2 seems unlikely; especially given that donor N Protein seropositivity has actually climbed dramatically since October, particularly among middle-aged adults. Thus, the UKHSA’s actual recent observations render the referenced “recent” observations false:
My guess? As “breakthrough” infections became normalized, the middle-aged Covid-vaccinated + infected in the UK became more likely to donate blood. Older donors may be more likely to drop out of the donor pool after infection (especially if infections are more severe); or they simply generate fewer N protein antibodies due to having a less agile immune system in general (a feature of aging which is, itself, construed in support of a real-world relevance to OAS, as discussed in “(Not) Coming Up”). And younger donors may still be sensitive to “ideological taboos” against breakthrough infection.
Elsewhere, in the OAS saga:
“Even-Steven.” (OAS is “proven” via generation of a more balanced immune response against Alpha or Delta after breakthrough infection.)
“Macaque Me an Offer I Can’t Refuse.” (OAS is “proven” via animal models where mRNA-vaccinated hamsters and macaques do better than unvaccinated controls vs Omicron.)
“Funeral for a Fact,” footnote 3. (OAS is “proven” because the boosters restore infection efficacy vs. Delta during the Omicron wave.)
“Darmok and the Spike Protein at Tanagra.” (OAS is “proven” when high pre-existing antibodies against coronaviruses… don’t correlate to severe outcomes in infection with SARS-CoV-2 in any way.)
The term was created to refer to limits in vaccine-induced, and thus artificial, manipulation of antibody motifs. Vaccination with A’ only results in the revived circulation of antibodies previously induced against A. It is the relevance of these limits to real-world infection outcomes that are a figment of the imagination. “Inability to vaccinate against A’ after vaccination with A” is not “inability of the immune system to respond appropriately to the virus bearing A’ after vaccination with A,” and it requires imagining that “the immune system = antibodies” to fantasize, by extension, that the two example statements would be equivalent.
As human understanding of the immune system has expanded beyond antibodies in the six entire decades since the term “Original Antigenic Sin” was coined, myriad other, more plausible mechanisms by which vaccination could interfere with immune response are available for us to fret over.
Namely, since the Covid-vaccines do not engage the natural site of infection, they cannot induce the normal suite of mucosal / cellular immune response that would follow natural infection. Since this is the most plausible explanation for why vaccine-induced immunity is inferior to natural immunity, the obvious “Big Question” is whether breakthrough infection corrects this mis-programming. If it doesn’t, that would be bad; and also incompatible with the narrow, primitive worldview of a lifelong failed-influenza-vaccine-developer in 1960.
It wouldn’t be “OAS.”
OAS is a myth.
These exercises include scientific papers for a reason.

See “Funeral for a Fact.”
Akkaya, M. et al. “B cell memory: building two walls of protection against pathogens.” Nature Reviews Immunology volume 20, pages 229–238 (2020).
For more on the highly altered tropism of Omicron, see, again, Whittle, Robin. “Omicron's generally less harmful mechanisms emerge.” (2022, January 6.) Nutrition Matters.
(link anchor)
21 October 2021 (pdf)
27 January 2022 (pdf)













It’s a shame he bounced you from his substack. This kind of back and forth is necessary. Thank you.
An interesting alternative opinion, thanks! We need more debate on this to seek the actual truth.
https://nakedemperor.substack.com/