The fall of the "Covid-19 was bacterial pneumonia" theory
Now it's *checks notes* toxins
Throughout the year, I have engaged in a one-way criticism of the bacterial pneumonia argument levied by Neil, et al., and published at Where are the numbers? So, I might as well comment very briefly on the latest update. The comments on linguistics in the first section of this post have relevance to my recent critiques of “alternate” theories for polio and to no-virus-ism generally.
Ultimately, however, there is nothing substantial which needs to be added to my previous examination of why the theory does not hold. Especially, the reader should see the previous post for my “positive” case for SARS-CoV-2 causing the illness known as (severe) Covid-19; it won’t be repeated here.
The new update:
In this, the theory has been rocked by a conversation with Pierre Kory and Jackie Stone, resulting in a significant reformulation without any admission of error (always a good sign of open-mindedness). Kory and Stone’s comments are wide-ranging, and cover many of the same points I made in my own, prior (one-sided) response, one of which is completely explosive of the bacterial pneumonia theory and others which are more supplemental, but still relevant.
Linguistics first, again
As before, I will first review the main supplemental point: Covid-19 was different than regular “pot-luck” pneumonia in aggregate.
This difference is just as women and men are different in aggregate. Some women and men might individually be similar; but anybody can instantly tell by the recorded qualities of a random sampling of either, which is which. Longer stays in ICU; Covid-19. Most common high-school sport football; men. But is football really “different” than track and field? Don’t both involve outrunning opponents, or throwing objects, or jumping? And aren’t only a minority of men actually playing football? This is just deconstructionism. You can do it for people, animals, plants, furniture, vehicles — almost anything. It is a feature of language, not of reality.
Any attempt to convince the reader that Covid-19 was merely regular pneumonia must elide the differences of Covid-19 by selectively highlighting ambiguous individual observations, and ignoring the big picture.
But, what is the actual premise explaining why this is a valid means of considering an infectious disease, even though it wouldn’t work for considering almost any other real phenomenon? Is it assumed that infectious diseases obey “special rules” — that they are not like people, cars, chairs? Infectious diseases, by some iron law discovered only by skeptics to be written in the fabric of the universe, must never have individual variation or contain qualities that overlap with each other; they cannot be discerned as an aggregate of qualities just like anything else is, in fact any aggregate observation is an illusion, per the iron law. If you find a chair with three legs, all chairs do not stop being chairs. But if you find an infected person without happy hypoxia, the infectious disease stops being an infectious disease? Why? What reason?
Of course, the answer to this rhetorical question is obvious: Because you can’t see infectious diseases with the naked eye. But the limitations of the human eye do not impose special rules on whatever is real; as such, they do not create special, positive restrictions for how we observe and think about infectious diseases, wherein the universal problems of epistemology and linguistics operate as magic solvents that literally un-create (as far as the skeptic is concerned) whatever we can’t see.
Neil, et al. of course previously argued both that Covid-19 is not different, and that any differences can be explained by the reaction to the virus. These two arguments are not compatible. If differences originated “from the reaction to the virus,” then the result was still that Covid-19 was different.
The latest bout: more linguistics, this time with hypoxia
Ironically, the newest post was originally published under the title “A closer look at Spikeopathy as the explanation for the novel symptoms associated with COVID-19” (since changed, though the url still shows the original). But immediately after interviewing two doctors who saw the disease up close, the authors flood the reader with clinical overviews from spring, 2020 — beginning with Wuhan. They seem to prefer to understand Covid-19 from far away. I might as well ask someone returning from France what the people are like, and then email them back the next day with a long set of examples in which the described qualities are shared by others. “In short, you have failed to convince me that French people are real.”
This leads to a feature which Kory highlights in the interview and which I highlighted in my previous response in August: Happy hypoxia. This is where Covid-19 was not only different, but distinct from regular pneumonias, in which hypoxia is accompanied by discomfort and conscious breathing effort. The mechanism of Covid-19 hypoxia — tricking the vasculature of the lungs into sending blood to airless tissue — is discussed in my August response.
Of course, the skeptical, linguistic approach could still counter that only a portion of patients with respiratory failure experienced this distinctive symptom. (Just as only a portion of men played football in high-school.) But asymptomatic hypoxia still totally demolishes the notion that Covid-19 was just regular pneumonia, and reveals Neil, et al.’s previous hyper-focus on radiology as naive (hypoxia wasn’t even mentioned in their August post).
And so a notable change occurs in the latest post, when addressing hypoxia, in that the authors are no longer quibbling over complex variation but deceiving the reader by omission. Kory is made to sound like he came up with the hypoxia observation in a fever dream:
In 2020 Dhont et al investigated the pathophysiology of ‘happy’ hypoxia in covid-19, noting that it occurred in around 20% of hospitalised patients, but the condition was also observed in patients with atelectasis, intrapulmonary shunt (i.e. arterio-venous malformations) or right-to-left intracardiac shunt.
In 2020 Laredo et al failed to find any strong evidence of happy hypoxia: […]
As did Plummer at al in 2022:
This brief overview hardly corresponds with the general tone of the literature. Even Dhont, et al. says:
The disconnect between the severity of hypoxemia and the relatively mild respiratory discomfort reported by the COVID-19 patients contrasts with the experience of physicians usually treating critically ill patients in respiratory failure
I.e., physicians like Kory.1
What of the other two references? Both of these fail to apply a rational definition of happy hypoxia. Laredo, et al. firstly only reports vital figures on admission. The picture of what happened over the full course of disease is thus totally absent. It further uses breath rate to define asymptomatic hypoxia — but this improperly excludes patients who would have experienced compensatory hyperventilation without self-consciousness or discomfort. Plummer, et al. repeats this problem, using “respiratory rate, heart rate, systolic blood pressure, and temperature” as a proxy for physical distress.
Neither of these studies can measure clinical observations — (the absence of) the alarm and discomfort that normally comes with hypoxia, but which is primarily regulated by CO2 rather than oxygen. These patient characteristics are what Kory and others have described as being distinct in Covid-19.
Given the prior fondness of Neil, et al. for reports from the earliest months of 2020, why not quote, instead, from Oldani, et al.?
When SARS-CoV-2 began to spread in our country [Italy], we supposed we were facing an explosion of cases of interstitial pneumonia similar, from a pathophysiological perspective, to those induced by influenza viruses, cytomegalovirus or Pneumocystis jirovecii among others. We all had in mind patients in respiratory distress, with rapidly deteriorating clinical conditions that would require a quick referral to the ICU, where protective invasive mechanical ventilation, pronation, and even Extra Corporeal Membrane Oxygenation (ECMO) could be provided.
However, as soon as COVID-19 patients started to be admitted to our hospitals, we were all surprised to face completely different patients than expected. Most of them did not even complain of dyspnea. No sense of breathlessness, no rapid shallow breathing, no need for accessory muscles of respiration, despite devastating CT scan images or dramatically low PaO2/FiO2 ratios.
Bacteria theory destroyed — or not?
I begin with the motte — the linguistic argument. It is invincible because it makes an unreasonable demand for knowledge. “You have failed to convince me that French people are real.”
The bailey — the weak, but seductive argument — is and has always been the bacterial pneumonia theory. This brings us to the explosive point in Stone and Kory’s interview:
Stone: “We treated for bacterial pneumonia in the first half of 2020, and they still died.”
Kory: “Secondly, in ICUs most docs have a hair trigger for empiric antibiotics […] I saw a lot of antibiotics being used in patients in my NYC ICU in the spring - didn’t help.”
Me, in August: “Patients were given plenty of antibiotics, so it is nonsense to suggest they died from bacteria. (previously shown here).”
Here it is appropriate to quote from Neil, et al.’s summary of their theory back in August:
Summary
We have investigated the pneumonia hypothesis: that a proportion of covid-19 deaths, those with associated respiratory symptoms (rather than deaths coded as covid-19 because of a positive PCR test, that are absent symptoms), were caused by bacterial pneumonia, and that bacterial pneumonia was the primary, not the secondary, infection.
And where are the authors now?
Many/most covid-19 cases would have been ‘ordinary’ influenza and bacterial pneumonia cases.
Some were not viruses or diseases at all but caused by toxicological events.
Each of these were misattributed to covid-19 either deliberately or through a process of human error.
So, this is still, fundamentally, a motte and bailey stance. Bacterial pneumonia (which is impossible as a primary cause of death in a patient population smothered with antibiotics) is smuggled back in. Stone and Kory’s points are just ignored, as it is presumed the reader has forgotten them after so much distracting “what about the men who didn’t play football” study-quotation. Indeed, a safe presumption, judging from the comments — no one even brings up the point about antibiotics, nor seems to care that much about the specifics of what (if not Covid-19) sickened and killed people.
Toxicological events?
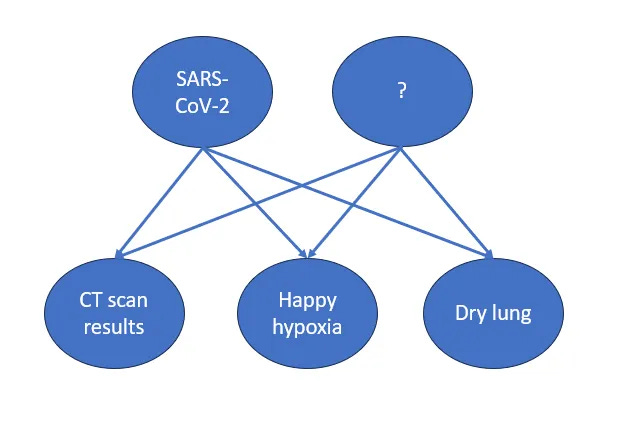
Yet the distinguishing clinical characteristics of actual Covid-19, as described by Stone and Kory rather than as willfully misinterpreted in papers about CT scans, have clearly impressed the authors that something besides regular pneumonia was at play. They produce this diagram to illustrate their puzzlement:
They clearly must hold onto the bacterial theory — “many or most” cases would have been regular pneumonia of bacterial or mysterious kinds. (So what if antibiotics did not work? Who really knows if bacteria usually cause pneumonia? Where are the numbers?) But a “something else” must now be allowed to sulk around in the playpen.
A reasonable theory and a far-fetched theory are offered.
The first, vaping, can be dismissed as irrelevant — based on age alone, it is safe to assume that most Covid-19 patients did not vape; most vape-ers did not experience relatively high rates of Covid-19. Vapes if anything should be suspected of protective effects absent further details.
The second theory is thus obviously necessary even though the authors are clearly reluctant to turn it over. Despite burying this theory at the bottom of their post, and declaring it a “low probability,” everything which has preceded it, that is to say the entire skepticism of SARS-CoV-2 as a novel virus causing a distinct disease called Covid-19, depends on it. And what is this theory?
[A] toxic poisoning event affecting, not individuals using e-cigarettes or vapes, but crowds of people in enclosed spaces. […] If someone was intending to release a pathogen that might mimic a respiratory disease, we might speculate that this might be more manageable in indoor spaces.
Well, ok. A “pathogen mimicking a respiratory disease,” which someone might want to release.
But then why wouldn’t that same person just use a virus?
If you derived value from this post, please drop a few coins in your fact-barista’s tip jar.
Asymptomatic hypoxia is apparently also common when acclimating to high altitudes; but this wouldn’t be commonly observed in most ERs etc.







What he said!
Thank you for so eloquently putting into words what I cannot! My simplistic way of explaining to my husband what the post that you refer to is about, can be summed up as two sides arguing
‘That car is red’ v ‘ No, that bike is blue’.
Why do people on ‘our’ side continue to tie themselves up in knots arguing over things that are not helpful. I used the above example as a reply to an Unbekoming post on whether viruses existed trying to clarify how I think the no virus people argue.
I can only hope that if there really is a secret cabal of evil-doers behind all this then they are all infighting and squabbling just as much and therefore their plans won’t come to fruition!
Thankyou for your work. Dr Kory/FLCCC wrote early on that he/they were seeing Organising Pneumonia possibly caused by hypersensitivity pneumonitis. Dr Kory stated that most doctors misdiagnose Organising Pneumonia, they aren't trained to see it on X-ray and have a default setting to antibiotics.
The hypersensitivity pneumonitis fits with the comments of South African Dr Shankara Chetty, who was highly successful with his early treatment program. Dr Chetty used antihistamines as part of his protocol, he said there was an allergic response to the Spike Protein.