Decoding Polio
A theory of polio as a "needle-borne plague."
Post status: Withdrawn / archival
Please see the revised and improved explanation for the polio mystery here:
Spacer:
Archived post:
[T]here is much about the disease that remains a mystery. One of the ironies of the great polio crusade waged in the middle of the twentieth century is that its crowning achievement — the successful vaccines of Jonas Salk and Albert Sabin — helped close the door to future research. […] Questions and problems that had swirled about this once-terrifying disease now seemed beside the point, almost arcane.1
I Can’t Believe It’s Not Lupus
In my faded memory, all but the last 5 minutes of every House episode are spent displaying the many moving parts of the mystery; and by the time said mystery is solved the viewer doesn’t even remember half the parts.
A House treatment of polio would require an entire season for the same basic exposition. The disease — symptomatic, observationally epidemic paralysis — is vastly more mysterious than most realize. This goes both for vaccine worshipers, who are usually unaware that asymptomatic infection and transmission were widespread even at the height of paralytic waves, and vaccine skeptics, who have a limited familiarity with the evidence for viral etiology. But as “a whole House season”- worth of explaining why polio is so mysterious would take weeks of work to accomplish, and probably wouldn’t be read by anybody anyways, I will skip to the scene where the answer rush-limps to save the patient in the nick of time.
Disclaimers:
1. Is this really a novel theory?
A good solution to any mystery should seem obvious in retrospect. That is the case with my new theory for polio, which struck me last night and immediately felt like a fact I had known all along. Once you have all the pieces in place (which, again, takes forever), the solution is obvious.
As such, my standard Crackpot Disclaimer applies: I do not do much “secondary source” reading, meaning reading of the work others have done to synthesize prior biological research. It is thus entirely possible that someone else has already published this theory before, and I am just unaware of their work. If so, apologies for unintentional plagiarism.
This theory does, however, owe partial inspiration to the work of HV Wyatt in laying the case for an auto-immune, provocation-based etiology for symptomatic polio in the 70's.2 In particular I wish to acknowledge that Wyatt — who remarked on the influence of injections on polio outbreaks in Africa — may have already proposed the same solution I offer here, in work I have not read.
2. Yes, I have read Dissolving Illusions
In short, the theory advanced for polio in that book is not compelling. Readers familiar with the book should understand that in advancing a “It was all the braces, and then DDT” theory, Illusions downplays the embrace of the Kenny treatment in American polio care circa 1940-43,3 and does not account for rapid-onset, limb-specific muscle atrophy (which cannot be explained by either braces or an inhaled, chemical neurotoxin).
In general, Illusions extrapolates from the evidence of widespread iatrogenic exacerbation of polio, to somehow imply that treatment for polio caused 100% of polio in the first place, including by time-travel if necessary.
It is certainly clear that many medical interventions worsened outcomes; but to explain how these interventions compounded without causing paralytic polio in the first place — which is the whole reason these harms went undetected at the time — is a more challenging feat. That is what I have done here.
3. This could be a dead end
My polio theory is testable in two ways, and as such may be disproven or may have already been disproven, unbeknownst to me.
Medical records may still exist from 1880 - 1954 to verify or falsify sequential injections.
Abortive neural invasion may be contradicted by experimental evidence (though, the current experimental evidence is a mess, largely owing to the necessity of working with neurotropic strains in the early era, diminished resources in the modern era, and the elusiveness of the world of intracellular immunity in vivo).
However, even if this whole theory blows up, it will hopefully make for an amusing read, akin to the solve on a House episode.
Polio: The Needle-Borne Plague
Graphical abstract (note — again, the etiology here will soon be scrapped as in the note at the top of this post):

The first recorded polio epidemic in the United States occurred in the Otter Valley, near Rutland, Vermont, in 1894.4
I. Polio before hypodermic needles.
Paralytic “polio” is a (possibly) ancient disease reflecting a rare outcome of natural (enteric) polio virus encounter. “Epidemic” polio — multiple coincident occurrences of paralytic polio with or without transmission chains in a given region — did not exist before hypodermic needles, and was still a rarity before the popularization of injection with anti-toxin for diphtheria, in 1894.
Note: "Vaccination," as in vaccinia inoculation for smallpox, involved dermal scraping, and thus played no role in the advent of medically-injected polio virus.
II. Polio after hypodermic needles, 1881 - 1910.
Epidemic, paralytic “polio” is a byproduct of the medical invention of hypodermic needle injection in the mid-1800s, followed by the advent of anti-toxins for diphtheria and tetanus and expanding injection of children with the same in the 1880s.
Anti-toxin injection was a nascent practice in the 1880s, limited mostly to tetanus treatment. Instead, increasing generic use of hypodermic needles in medicine, including pediatric medicine, likely contributed to the first, smaller European outbreaks from 1881 (Sweden) to 1893, the largest involving 44 cases (again in Sweden).5
Use of diphtheria anti-toxin exploded in winter of 1894, the year Behring and Kitasato’s serum was commercially imported in the US.6 This year is also the turning point for observed epidemic polio outbreaks.7

In the US and Australia, no observed epidemics preceded 1894:


III. Why diphtheria anti-toxin; why children.
By the aughts of the 20th Century, “injection as medicine” was rampant. The scene on the ground must have been indistinguishable from a play-through of BioShock: Experimentally or in practice, doctors in 1907 and 1908 alone self-reported injecting everything from olive oil,8 to atropine and strychnine,9 saline,10 delicious cocaine,11 meningococcus vaccines for acute meningitis,12 typhoid vaccines for travel,13 and literal air.14
None of these appear to have been as frequently targeted toward children as diphtheria anti-toxin. Further, severe cases in one child may have increased the likelihood of injections into siblings, explaining the intermittent observation of intra-household paralytic polio cases that might be observed the following summer (emphasis added):
The case of Janet G. may almost be said to have the value of a controlled experiment in view of the fact that her sister, Maud G. age 5 (Ref. xv. 20), and her brother Thomas G. age 8 (Ref. xi. 92) were received into hospital each with a first attack of diphtheria on the same day and at the same hour as Janet G. was admitted with her second attack of diphtheria. In all three cases the faucial appearances were approximately similar: the sisters were equally affected; the membrane in the boy's throat was somewhat more extensive. In all three cases anti-diphtherial serum was administered at the same time: each of the sisters received 27 c.c. whilst 36 c.c. were given to the boy.15
The same paper also demonstrates the propensity for diphtheria treatment to result in multiple injections in the same patient:
When 21 days had elapsed from the first injection of serum a recrudescence of diphtheria occurred, and the patient received a second injection of anti-diphtherial serum, again into the subcutaneous tissues of the abdomen
This does not mean that, when it comes to multiple injections, diphtheria anti-toxin was most-likely-to-offend on a per-case basis. A case-study of treatment for meningitis in the same year, for example, describes the administration of 11 lumbar punctures, 6 injected meningococcus vaccines, and at least one injection of strychnine and ether.16
Rather, it is on a per-population basis that the diphtheria anti-toxin was the likely “injection of first resort” for childhood illness, in the aughts of the 20th. No other childhood disease was as lethal and as amenable to injection at the time; and early (quasi-pre-symptomatic) recommendation of injection was considered prudent for children under four. In a 1907 paper (emphasis added):
We must distinguish between, first, those of tender age, under 4 years, and, secondly, the older children and adults. In the first case the use of prophylactic antitoxin is relatively more important from the fact that on such the action of the toxin is more severe, and the diagnosis of an attack is a more difficult matter, with greater risk if there is laryngeal development.17
Compared to Batten’s description of the incidence of polio in the same era (emphasis added):
The incidence of the disease [paralytic polio] on young children is a constant feature, and it commonly falls upon children during the second and third years of life. Babies in arms are rarely affected; as the age advances the incidence rapidly declines. In the [1907 - 1909] Massachusetts epidemic of 440 cases under 6 years of age, 304 occurred in children between 1 year and 4 years old.18
IV. The impossibility of polio-free injections (of any type).
Given modern understanding of (pre-“eradication”-era) polio virus as a ubiquitous environmental companion (akin to the related rhinoviruses that are implicated in the common cold), or “contaminant,” and the obvious inefficacy of antibacterial sterilization of needles on viruses, it is in fact impossible that needles did not routinely inject live, environmental polio virus, even in the winter (when diphtheria anti-toxin was used).
Such low levels of environmental polio virus would also have routinely entered the gastrointestinal tract, even in the winter.19 However, outside of seasonal summer surges, these passages of virus would not have been in the dose required for asymptomatic or symptomatic “infection” resulting in generation of a mucosal and humoral memory immune response. Polio, before “eradication,” is like the woods: They are always around, but children are only immersed in them in the summer. And so the contents and surfaces of needles in the winter would still not be free of surrounding polio virus (especially if the contents had been prepared in the previous late summer anyway).
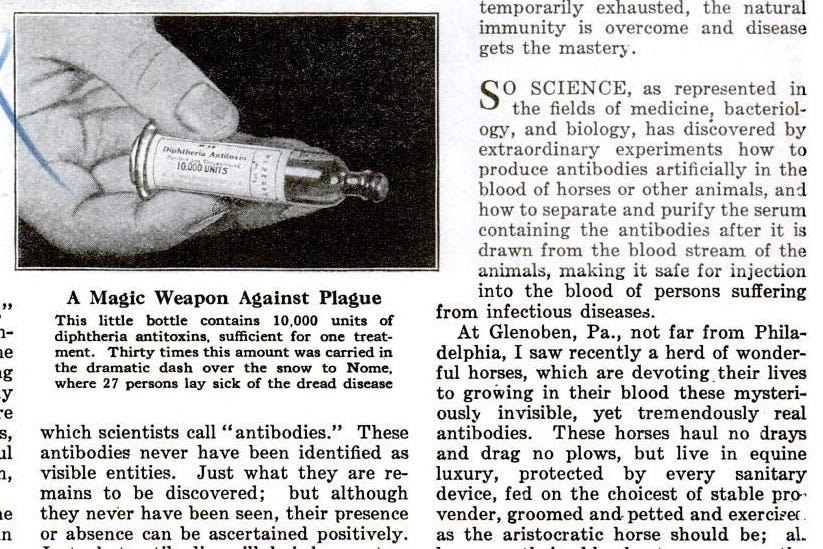
The following, modified illustrations from a 1925 article in Popular Science should demonstrate the likely sources of polio contamination without and within diphtheria anti-toxin injections:



There is no question that diphtheria anti-toxin injection introduced live polio virus into the abdomen of children; nor that injection with anything in non-wild-polio-“eradication” regions introduces polio virus.
The question, answered in my abstract above, is what happens afterward.
V. Proposal: Abortive neural infection sans adaptive immune response.
My theory proposes, first, that injections in the pre-“eradication” era were routinely contaminated with live polio virus of one of the three serotypes. This is essentially axiomatic: Polio virus was everywhere; it would have been on needles and within their contents.
The second proposal, more speculative, concerns the results.
Individuals, namely older children and adults, with pre-existing immunity from natural (enteric) polio virus encounter would have enough circulating antibodies and Memory B Cells to inhibit invasion of neurons by injected polio virus.
Young children would routinely lack neutralizing antibodies to injected polio virus.
Injected polio virus, due to affinity for the CD155 receptor, would be taken up by a few immune cells and by neurons near the injection site. The diphtheria anti-toxin was commonly injected into the abdomen:
Antitoxin should always be injected and never given by the mouth, either side of the abdomen being the most suitable site. 20
Thus, the most affected nerves for injected polio in non-immune children would be the in the side of the abdomen, followed by the legs. Involvement of pulmonary nerves (back at the other end of the circulatory cycle) may simply reflect greater fragility of these nerve fibers and connected muscles in children.
Given that paralysis / polio was not one of the recognized, acute symptoms resulting from diphtheria anti-toxin contamination,21 invasion of nerve cells must have been self-limiting. Therefore, polio infection was likely innately suppressed.
Neuronal immunity is primarily innate-mediated (for example, the brain is one of the body’s immune-“privileged” zones22). The innate, intracellular immunity mechanism for suppression of viral replication in neurons is the formation of amyloid plaques. These act as firewalls which prevent the transmission of viruses to other neurons.
Injected polio thus likely leads to innate-arrested (abortive) neural invasion without the formation of an adaptive immune response.
VI. “Ordinary” / Sporadic polio: A quasi-unnatural viral disease.
Notwithstanding spurious interpretations of a lone, throwaway hieroglyph, the localized limb-specific “wasting” of “ordinary” polio is sui generis. In rates that accord with childhood viral illness, it doesn’t happen in animals; it didn’t happen before hypodermic needles; it hasn’t happened since the “eradication” of polio afterward.
At best, it was as scarce as the rarest of genetic disorders manifesting in children today, apparent only in the one Walter Scott in a given region in a given generation, and even then not matching the etiology later observed after hypodermic needles.23
There is therefore no reason to suppose that “limbs suddenly turning into sticks” is in any way a natural viral disease.
Wasting of limbs is often interpreted as an disuse-mediated effect of neural damage. In fact, it is a result of a unique atrophic syndrome caused by the annihilation of muscle tissues and subsequent replacement with useless fiber and fat. This may be due to immune-mediated destruction of muscle tissue, or over-sensitization of muscle to background levels of neurotransmitters, due to the “turning off of the lights” of the feeding neurons (denervation), leading muscles to “twitch themselves to death.”
In muscle the most obvious features of denervation, according to Solandt, are physiological fibrillation [spasm], changes in electrical and chemical excitability, and, later, atrophy. The first three are probably correlated, one essential feature bing that the muscle becomes hypersensitive to acetyl-choline so that it will react to concentrations normally present in tissue and blood with resulting [spasm]. This [spasm] begins on the fifth day and may persist for several weeks. The atrophy which subsequently occurs in muscle following denervation is a loss of weight chiefly in the contractile elements or fibrils of the muscle fibres, with a later absolute increase in connective tissue. […]
In the muscle supplied by the destroyed neurons after the initial [spasm] the essential lesion is a primary atrophy. This is soon accompanied by an increase in the pre-fascicular connective tissue, and later the complete atrophied muscle is filled in either by fibrous tissue or fat. Secondary atrophy may occur in healthy muscle fasciculi which are cut off as islands in a sea of fat or in other healthy muscle fibres as a result of disuse.24
Other accounts of the usual course of disease instead evoke simultaneous destruction of nerves and nearby muscle tissues (emphasis added):
As to symptomatology, the subcommittee saw no reason to depart from the former conception of the disease as one in which “the paralysis, however widely distributed or however narrowly limited, and in whatever part of the body, comes on after an acute onset marked by fever, vomiting, and convulsions.” Moreover, “the paralysis is associated at an early date with atrophy, with changes in the electrical reactions, and with a loss of reflex activity in the paralysed parts.”25
In either case the muscle destruction is not a result of disuse, but a more direct “collateral” harm from the destruction of the nerve. As no other neurotropic virus — whether influenza, chicken-pox, or rabies — results in the similar wholesale denervation of limb muscles, this would not seem to plausibly result from direct damage to neurons by polio virus.
For this reason, my theory proposes a pseudo-auto-immune26 mediated destruction of nerve fibers servicing limb muscles, due to sensitization to remnant polio proteins left over from abortive infections of injected environmental polio virus. T Cell and antibody-mediated cellular immune attack of quiescent polio-infected nerves results in collateral destruction of the entire nerve fiber and of the serviced muscle, or nearly-so. Alleviation of denervation-induced muscle spasms, according to the Kenny method, may have reduced muscle fibrosis and atrophy in cases where no acute auto-immune attack of muscle cells (myocytes) occurred.
VII. Fighting fire with kerosene: Lumbar puncture, generic injections, penicillin (polio-coincident polio injection).
After 1894, another turning point, at least in the US, came in 1907. This may not coincide with, but certainly seems to reflect the transition to aggressive employment of lumbar puncture as a “diagnostic” tool, especially in the Northeast and in Flexner’s New York. This trend appears to culminate in the disaster of 1916.
Despite the absence of any clinical insights which could lead to improved treatment and better outcomes (short of ruling out other infectious agents), children who were brought to doctors with “polio-like” symptoms (fever, vomiting, and especially stiffness) were subjected to lumbar puncture, with no clear threshold for mildness or severity of initial presentation. Likewise, arbitrary decision-making seemingly attended all the other injection-based “treatments.” As Wyatt summarizes, of the 1916 super-epidemic (emphasis added):27
The nearly nine thousand cases in Greater New York were treated in the four New York City hospitals and in 27 others [4]. Almost half,28 4516 (of which 3083 were given symptomatic treatment and 956 had a lumbar puncture) were treated in the City hospitals [...]
The disinfectant hexamethylamine (urotropin) was used not only externally, but also as an internal disinfection: after intravenous injection, it appeared in the spinal fluid. It was given to 51 cases by intraspinal injection every six hours
The rationale for giving tetanus antitoxin was that tetanus, rabies and poliomyelitis all attacked nerve cells, so perhaps giving the antitoxin would block access to absorption sites on the cells [6, 7]. But the giving of diphtheria antitoxin to five cases with three deaths was ‘a most unwarrantable procedure [with] no good results.’
Adrenaline was injected intraspinally, but there were 100 cases with 45 deaths although Meltzer claimed that it aided recovery [8]. It was also given intramuscularly, although of 35 cases, 23 died. Quinine and urea hydrochloride were given intraspinally: three of six children given many doses by mouth and intramuscularly died.
Fischer at the Willard Hospital reported on several hundred patients, saying that lumbar punctures should be done and blood transfusions given if the patients were emaciated. Five cases were given intravenous salvarsan ‘with excellent results’. Deep intramuscular injections of strychnine (given as a tonic) were given three times a day on alternate days. He gave 10-15 cc of convalescent serum if possible [9]. Fischer noted that ‘a severe febrile reaction frequently follows the intraspinal injection of human serum. In some case nausea and vomiting followed’. He also gave intraspinal irrigations with normal saline after withdrawing 30-100 cc of CSF
Barber in a lecture in 1915 […] suggested giving strychnine internally or subcutaneously
It was thought that normal (adult) human serum neutralized the poliovirus and was employed in 114 cases, intraspinally or intramuscularly.29 In one instance, 23 cases were given the serum, but 15 died. Convalescent serum was tried with nine cases injected into the spine and six into the muscles.
Further, regarding lumbar puncture alone and in combination with other spinal injections:
LP was commonly used and by itself in 956 cases in the City hospitals. At one hospital there were 209 single punctures to relieve severe meningitis or hydrocephalic symptoms and 119 with multiple punctures: 121 died. In another hospital 43 were treated by spinal puncture of whom 17 died. At Riverside Hospital however, 156 cases received lumbar puncture and only 21 died. [Note: Disparities in aggravation rates by site are consistent with contamination with environmental polio virus.] Adrenaline was also given with LP in 100 cases: 19 cases were given intraspinally and 10 died. Meltzer of the Rockefeller Institute, after withdrawing fluid by LP, injected two cc of adrenalin every six hours for four days [8]. Removal of fluid calmed the patient and perhaps took away some poisons. However, in some hospitals, spinal fluid was given back by intramuscular auto-inoculation to 27 cases, of which 15 died.
Hair-trigger injection of pre-paralytic cases seems to have contributed to the polymorphic manifestation of the disease in the 20th Century, where one form — the “ordinary,” limb-stick kind — is a novel outcome resulting from priming by injection for other medical reasons, and the other forms are formerly rare, Central Nervous-System-centric outcomes resulting from coincident injection of polio virus during mild illness.
A review of the 1908 epidemic in New York characterizes both these “other” forms — cerebral and neuritic — as sudden-onset, implying no influence of lumbar puncture or iatrogenic intervention in general.30 However, the birds-eye-view strongly supports an increase in CNS destruction during seasonal polio infections resulting from treatment-induced lumbar punctures. The overall impression is that New England, followed by other regions of the US and elsewhere, suffered a holocaust of medical panic- induced paralyzations between 1907 and 1916.
The case for aggravation of paralysis due to (clinically useless) lumbar puncture went little-examined until the 50s. Wyatt writes:
The taking of CSF by lumbar puncture from suspected cases of poliomyelitis was, however, a controversial technique in the early 1950's. Two French experts, Debre and Thieffry, advocated routine LP and examination of the CSF for the diagnosis of acute and non-paralytic polio and to differentiate polio from Guillain-Barre syndrome [14].
Mollaret, however, compared the progress of patients who received lumbar punctures after the onset of paralysis with those without paralysis [15]. Of 17 who received lumbar punctures on the day of paralysis or the next, all had 'aggravation' of paralysis within 12 to 24 hr and 15 developed respiratory problems at the same time or a little later. Ten patients with clinical signs, but no paralysis, were given lumbar punctures and all developed paralysis 12 to 48 hr after and seven developed respiratory problems. One patient in each group died.
Mollaret quoted other cases and showed that if virus was inoculated into monkeys and paralysis did not occur, then a lumbar puncture made subsequent paralysis more likely.
In a 1954 review of provoking and localising factors in polio, Trueta and Hode, from Oxford, England, wrote of 'the potential damaging influences commonly used in medicine, among the most potent are spinal puncture ..' [17] : they did not elaborate. […]
By definition, provocation occurs when infection and injection overlap, with paralysis following 7 to 28 days later. Intramuscular injections (IM), exercise and child-birth in the 24-48 hours before paralysis occurs, result in more severe paralysis of the regions concerned and are called aggravation [19]. The enhancement of paralysis 12 to 48 hours after LP [2] suggests that because the virus must be already in the spinal cord, this may be aggravation and cannot be provocation.
This “medical panic” that resulted in 1916 seems to have subsided in the early 20s, perhaps as a result of the waning of “diphtheria anti-toxin mania” leading to fewer polio outbreaks in the following summers. In fact, the aggressive promotion of the diphtheria vaccine, after the 1921 outbreak, may have paradoxically reduced the winter-time injection of live polio virus into polio-naive children (either due simply to the lesser incidence of repeat-injection in individual children, under a vaccine regime, or indeed to polio contamination usually occurring during pre-winter antitoxin preparation rather than “on the needle” in winter injections). By the late 20s, per-100k polio rates were on the rise again; followed by a building surge after the advent of (injected) penicillin in 1944:
Oshinsky, in Polio: An American Story, (inadvertently) describes how penicillin may have inadvertently re-animated the scourge of iatrogenic, coincidental polio-injection (emphasis added):
In the plague year 1952, horror stories abounded. On Tuesday, July 22, 16-year-old Catherine Thiel came down with a fever. She had spent the day on her farm in Mapleton, Iowa, doing normal chores in the blazing sun. The family doctor arrived, gave her a shot of penicillin, and recommended ice packs for her throbbing head. Catherine seemed to rally; her fever went down, her appetite increased. But two days later, the telltale signs appeared: muscle ache, joint pain, a stiff neck. The doctor returned. His diagnosis: polio.31
VIII. Why some older children and adults; why OPV and IPV protect.
The “three paths” of polio encounter available after the advent of hypodermic needles would be potentially taken for all three serotypes of wild polio.
For children, diphtheria antitoxin injection would make it likely (on a population scale, if not individual) that injected environmental polio would be encountered before enteric infection with the wild virus (leading to protective antibodies).
The result: Neuronal infection by injected, live polio virus, of the abortive (innate, intracellular, neuron-inhibited) type — with viral remnants leading to priming of later enteric polio-infection and auto-immune-mediated neural destruction.
For older children and adults, it was likely in the dawn of the Injected Medicine Era that natural infection had already generated protective antibodies which would inhibit neuronal infection of injected, environmental polio. Summer epidemics of paralytic polio thus did not chase inadvertent injection of environmental polio virus in older children and adults, in most cases.
However, some older children and adults would still lack humoral immunity (neutralizing antibodies) to one or two of the three serotypes. These would still be vulnerable to priming with environmental polio-virus upon medical injection; followed by later infection-induced auto-immune nerve destruction resulting in symptomatic, paralytic polio.
Widespread protection from injected live polio can only be accomplished by means of one thing: Widespread adaptive immunity to polio in advance of live injection, either by natural (enteric) polio infection or artificial (injected, inactivated) immunization. The Sabin “attenuated” oral polio vaccine (OPV) most closely resembles the fortification garnished by natural infection in adults in the pre-hypodermic needle era. Injected, inactivated polio vaccines (IPV) are a surrogate, imitation version of this immunity.
It remains to be seen whether IPV-immunity prevents priming after later injection of environmental (wild or Sabin) polio. The pending return of transmitted polio in the US and elsewhere will put this to the test.
If you derived value from this post, please drop a few coins in your fact-barista’s tip jar.
Oshinsky, David. Polio: An American Story. (Oxford University Press, 2005.) Ch. 1.
Wyatt, HV. (1976.) “Provocation poliomyelitis and entry of poliovirus to the CNS.” Med Hypotheses. 1976 Nov-Dec;2(6):269-74.
McFarland, JW. “Kenny Treatment in Poliomyelitis: An Evaluation.” Cal West Med. 1944 Aug; 61(2): 76–77.
This evaluation of the Kenny treatment is based on a study of 280 cases of poliomyelitis which occurred during the years 1942 and 1943. We are well aware that this report cannot be a final estimate of what the Kenny treatment has or has not done, because not a sufficient period of time has elapsed. However, we believe there is enough evidence from the progress made thus far to give us a fair basis from which to draw our conclusions.
With few exceptions, these cases were treated at the Los Angeles County Hospital during the acute stage of the disease.
Of the 122 Kenny-method-treated cases rated as worse than “slight” during initial presentation, 21 (17%) are only rated as “fair” (13) or “poor/zero” (8) improvement at the end of observation, another 23 (19%) as “good.” Thus a third or so of worse-than-slight cases remain symptomatic even with prompt use of Kenny’s method.
Geiger, JC. (1943.) “Concerning Incidence of Poliomyelitis in California.” Cal West Med. 1943 Aug; 59(2): 152–153.
He pointed out that physicians at Stanford, California, Children's and San Francisco hospitals have been trained in the Kenny method, adding that a number of out-of-town cases have been brought here for treatment.
Ed. (1943.) “Fact and Fancy in Poliomyelitis.” Br Med J. 1943 Jul 31; 2(4308): 141–142.
Regarding (and bemoaning) the enthusiasm for her method and her theories of etiology among some trained doctors.
Kenny’s intuition that CNS symptoms are not the primary cause of paralysis, and that the “action” is occurring in the affected limb, seems vindicated by later research, and indeed parallels Wyatt and my theory of an autoimmune response.
(Oshinsky, David. 2005.) Ch. 1.
Batten, FE. (1911.) “The Epidemiology of Poliomyelitis.” Proc R Soc Med. 1911; 4(Sect Epidemiol State Med): 198–226.
Bakalar, Nicholas. “A Diphtheria Cure, 1894.” (2010, May 11.) The New York Times.
Whether diphtheria anti-toxin is actually implicated in the 1894 polio outbreaks in Vermont (132 cases), Massachusetts (10 cases) and Australia (14 cases), is hard to ascertain. These may have been coincidentally large outbreaks seeded the previous winter by generic injections or locally-sourced diphtheria anti-toxins. There may be a locally-prepared prophylactic injection campaign of some type still in the historical record somewhere to account for the Vermont outbreak. At the same time, it is just as plausible that outbreaks of this scale were at the time, without widespread use of diphtheria anti-toxin, already common, and only the peculiar energy of Charles Caverly resulted in the coincidental documentation of the cases in Vermont in 1894.
The timeline in Europe, with polio cases exploding in 1895, more naturalistically fits a “diphtheria anti-toxin turning point,” as injection in winter, 1894 seeds paralytic polio cases the following summer.
Ed. (1907.) “Olive Oil Injections in Constipation.” Hospital (Lond 1886). 1904 Oct 22; 37(943): 68.
Strangman, MSP. (1907.) “Morphinomania Treated Successfully With Atropine And Strychnine.” Br Med J. 1907 May 18; 1(2420): 1173–1174.
Hay, AG. (1907.) “The Treatment of Sciatica by Means of Saline Injections.” Glasgow Med J. 1907 May; 67(5): 352–357.
Ed. (1907.) “On the Sensibility of Abdominal Organs and the Influence of Injections of Cocaine upon It.” Atlanta J Rec Med. 1907 Apr; 9(1): 42–44.
Mackenzie, H. (1907.) “Clinical Remarks On A Case Of Cerebro-Spinal Meningitis Or Spotted Fever Treated By Lumbar Puncture And Vaccine Injections: With Recovery.” Br Med J. 1907 Jun 15; 1(2424): 1407–1408.
Ed. (1908.) “Anti-Typhoid Vaccine.” Hospital (Lond 1886). 1908 Feb 22; 43(1121): 548.
Gubb, AS. (1907.) “Subcutaneous Injections Of Air As A Means Of Relieving Certain Painful Manifestations.” Br Med J. 1907 Nov 9; 2(2445): 1297–1299.
Currie, JR. (1907.) “Examples of the Immediate and of the Accelerated Reaction following Two Injections of Anti-diphtherial Serum.” J Hyg (Lond). 1907 Jan; 7(1): 61–64.
Peters, OH. (1907.) “The Limited Value Of Diphtheria Antitoxin As A Prophylactic.” Br Med J. 1907 Oct 5; 2(2440): 865–867.
Ward, R. Sabin, AB. (1944.) “The Presence of Poliomyelitis Virus in Human Cases and Carriers During the Winter.” Yale J Biol Med. 1944 May; 16(5): 451–459.
Poliomyelitis virus has been isolated during a cold winter from the intestinal contents of two patients with poliomyelitis, one paralytic, the other non-paralytic, and from a healthy sibling of each case. The existence of winter poliomyelitis, suspected on clinical grounds, is confirmed. The epidemiological implications which suggest themselves are: (1) Poliomyelitis may occur throughout the year, but its greater incidence during the summer and fall months may be related to opportunities for wider dissemination of virus. (2) It would seem possible that poliomyelitis, like typhoid fever and dysentery, may be transmitted by any of the several methods whereby infective particles derived from human excrement find their way to the susceptible human host. (3) At present the patient and the healthy carrier may constitute reservoirs of virus during inter-epidemic months.
As this is still in the era of “culturing” polio via inappropriate (non-chimp) primate challenge, Ward and Sabin would only have been observing the tip of the iceberg of highly concentrated virus, rather than true environmental ubiquity.
On the other hand, sewage PCR only reveals the viral dynamics in the post-Sabin-vaccine era.
I should look for a cell-culture, pre-vaccine (1950-54) era investigation of winter polio prevalence…
Miller, JW. (1906.) “The Treatment of Diphtheria.” Hospital (Lond 1886). 1906 Aug 4; 40(1037): 313–315.
For further discussion, see “It's Probably Not an Alzheimer's Virus.”
Walter Scott was born in 1771, the high era of injection-disfavor (1660-1860), and before the advent of Jenner’s dermal vaccine (1802). The illness leading to his lame leg struck at 18 months of age. It requires pure speculation to suppose that the 18-month-old Scott experienced rapid-onset atrophy as opposed to simple, acute neural or muscular insult resulting in suppression of later development. 18-months-old is simply too young to demonstrate the rapid atrophy unique to sporadic polio.

Ed. (1943.) “The Expanding Pathology of Poliomyelitis.” Can Med Assoc J. 1943 Jan; 48(1): 57–58.
Ed. (1911.) “Epidemic Acute Poliomyelitis.” Br Med J. 1911 Jul 8; 2(2636): 80–81.
Although the immune system is attacking self-cells, it is not (at least at the onset) due to sensitization to “self-antigens,” per my theory. However, secondary sensitization may result, as is commonly supposed for many apparently virus-induced auto-immune conditions (e.g. Guillain-Barre, etc.). Thus it could be the case that the aftermath / debris of the destruction of nerves prompts incidental sensitization to nearby muscles, leading to a positive feedback loop of auto-immune destruction.
Wyatt, HV. (2014.) “Before the Vaccines: Medical Treatments of Acute Paralysis in the 1916 New York Epidemic of Poliomyelitis.” Open Microbiol J. 2014; 8: 144–147.
This would seem to be just more than half…
Adult serum in fact would have commonly contained antibodies against one or all three types of polio virus; this would have been irrelevant in protecting against cellular immune attack of nerve cells that were already injection-“primed” well before enteric infection.
Ed. (1909.) “Acute Poliomyelitis in New York.” Hospital (Lond 1886). 1909 Jul 31; 46(1199): 459–460.
(Oshinsky, David. 2005.) Ch. 10.







As regards your theory, I do not have the education or training to discuss it. What I can say is that I'm always shocked and grieved by how confident "medical science" is with itself, especially when it uses children as lab rats. 😠
Very interesting and makes a lot of sense. Now AFM is also iatrogenic.
Injections and acute flaccid myelitis: the dog that hasn't barked
https://www.bmj.com/content/363/bmj.k5246/rr
Iatrogenic damage is incalculable.
Vaccines and Biologics injury table based on mechanistic evidence – Feb 2020 Covering over 125 conditions
https://doi.org/10.5281/zenodo.2582634