Explaining Polio, pt. 1
How injections promote central nervous system invasion during polio infection.
Polio series table of contents:
Summary:
Polio epidemics were outbreaks of paralytic illness caused by an increase in latent susceptibility to seasonal polio viruses among those who had not yet acquired natural immunity — this is essentially an axiom, given that the virus had always existed, but epidemics began to be noticed as more people suddenly experienced paralysis in reaction to it. This latent susceptibility was increasing across all ages, but younger children were at all times the least immune (previously infected) to polio and thus the most likely to experience infection for the first time, revealing their susceptibility to paralysis.
This increase in susceptibility, axiomatic but seemingly unexplainable, was due to the novel medical practice of needle injections, which were barely used before the late 1800s, and still barely used in children, until the advent of diphtheria anti-toxin and diphtheria vaccination. These two landmarks — 1893-95 and 1913-1926 — combine with the advent and expanded availability of (injected) penicillin in 1944-54 to drive the greatest increases in pediatric injection and thus explain the major geographic and historical trends of the polio era.
What is different between this theory and the default understanding?
The default understanding acknowledges, or at least acknowledged in 1950 and for the remainder of that century, that recent injection increases the incidence of paralysis upon polio infection, and influences which limb is affected, both in the human clinical setting and in animal models. This does not, however, contend that more remote (less recent) injections can increase incidence of polio paralysis, or more importantly that injections as a (novel) medical practice were responsible for the emergence of polio epidemics to begin with — even though there isn’t really another explanation. Essentially every statistical study into the problem concluded that there was “no evidence” that remote injections increased paralysis risk, which meant that most cases of polio still must have not been caused by injections at all.
This theory first pursues a simple circumstantial argument: Countries which injected children with things had polio epidemics. More injections led to more cases. Secondly, it will be shown that limitations to statistical investigations on less-recent injections served to obscure the longer-term ability of injections to increase polio paralysis incidence. The conclusion which must be reached is that the polio era was mostly caused by injections in medicine.
Pt. 1 (this post) will discuss the etiology of what is known as “provocation” polio.
This post will frequently refer back to the “mysterious” agent causing increased susceptibility to polio, as it would often otherwise seem that the needle theory is imposing logical burdens which in fact must exist no matter what was causing polio epidemics to increase.
i. What is the polio problem?
The polio problem is extensively described in a previous post. It is nevertheless essential to include a brief review here.
In short, there seems to be a lack of satisfactory explanation, within the official narrative, for why epidemic polio paralysis began to affect different countries in the global north at the turn of the 20th Century. Key to this problem and the lack of explanation for the same is that these same cases of paralysis mostly, or nearly always, depending on location and time, follow infection with the polio virus — they are not some outburst of poisonings from apples, or whatever one wants to dream up — and yet the same virus had always existed in man and was ubiquitous in the tropics, without previously causing epidemics.
To quote, again, from the frequently excellent JR Paul, writing in 1954:
Since 1900, and with increasing rapidity, epidemics of poliomyelitis appeared in Europe, North America, and elsewhere. Areas and approximate dates where and when this transition began are: Scandinavia, 1860-1890; western Europe, 1880-1890; the northeastern section of the U.S.A. in the 1890’s; and the southeastern section two decades later. From a comparative curiosity, infantile paralysis had become a periodic scourge. And once epidemics of poliomyelitis have begun to appear in a given region, the pattern has not been reversible. Furthermore, there has generally been a sharp or gradual progressive increase in prevalence, as measured over ten-year periods. In some countries the annual number of cases has risen over the past 20 years, as in the U.S.A., Canada, and France; in others, the number of cases has maintained itself at fairly high levels during this period with widely irregular swings.
Still more recently, i.e., within the past 20 years, has this epidemic evolution of the disease come to pass in tropical and semi-tropical areas such as Puerto Rico, Hawaii, Malta, El Salvador, and the Island of Mauritius. […] [M]any tropical populations had not been previously aware of the endemic character of their own local poliomyelitis or of how common it was [as a year-round rare pediatric condition]. In certain places of this type, such as the Philippine Islands, the native disease only came to the surface when groups of foreigners, such as U.S. soldiers, entered the country as “susceptible immigrants,” and there these military populations acquired poliomyelitis at far higher rates than would have been expected in their homelands. This was noted in the Philippines as early as 1936 and subsequently, i.e., before, during and after World War II. Documented examples have also occurred in Cairo, Egypt; in India; and in French Morocco.1
Thus, at the climax of the polio era, European adults could no longer travel to foreign lands without risk of discovering that they, too had somehow become susceptible to polio paralysis (whereas back home, at least they weren’t so likely to be infected on any given year to begin with) — this was something that had never happened in the colonial era, or during the Crusades, even though the ecology of polio virus had likely always been similar, with more frequent exposure and infection in warmer climates. (Again, “What polio is not” refutes hygiene and transportation as alternate explanations for this change.)
Soon afterward, the polio vaccines scuttled the problem, by preventing natural infection — but this left unresolved and unanswered the question of why people had become and were becoming more susceptible to paralysis as a result of polio virus infections to begin with.
So what changed? What mysterious “force” was rendering different societies newly susceptible to a virus with which they had lived forever without noticing?
ii. The etiology of so-called “provocation” polio
Readers familiar with my previous putzing-about on the polio topic will immediately note a coup has taken place with regard to the details of etiology. Suffice it to say that a mountain of historical details were collected in my present research safari. This corrected certain deficiencies in my prior research, especially concerning anatomical findings in polio autopsies (this endeavor as a whole was put on the back-burner last year, to prioritize SARS-CoV-2). All of this “new” information refuted my own theory about latent infections, and left the orthodox model as the only satisfactory theory.
This segment will describe what is known about post-infection polio paralysis induced by unrelated injections into limbs.
Pt. 2 will discuss the question of whether this known phenomenon is in fact the solution to the polio problem.
In what way did injections increase susceptibility to paralysis upon polio infection?
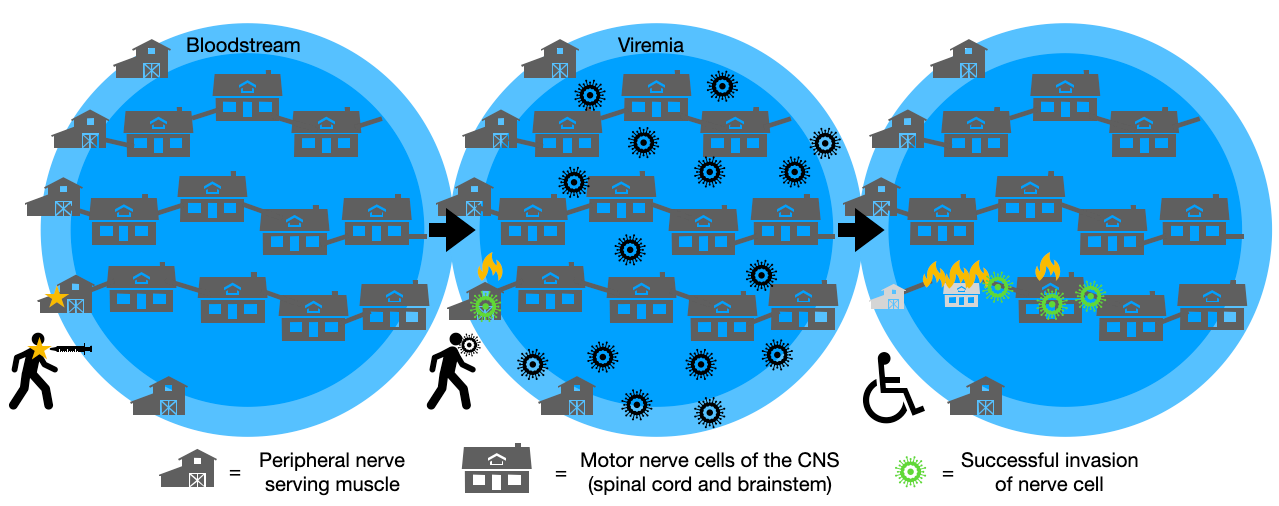
The simplest mechanism appears to be the one validated by (a handful of) modern experiments: In normal polio infection, the virus briefly appears in the blood stream before the arrival of antibodies. Normally it is not too likely to infect neurons to a great enough extent to result in noticeable long-term harm. The muscle “insult” and/or injury of injections increases both the incidence and velocity of destruction in the spinal cord as a secondary effect of viral invasion of nerves near the same injury. The virus soon afterward travels from these peripheral nerves upward along axonal connections to reach the motor neurons of the spinal cord. (When polio binds to its receptor in a motor nerve cell, it is whisked upward toward the cell body. This is “retrograde” axonal trafficking and ensures that the fastest path of travel for the virus is “toward the brain,” with the spinal cord and brainstem being invaded along the way.
This leaves out substantial still-unknown details, things one could theorize about. But overall it is a satisfactory explanation consistent with several pieces of research.
Human studies
From 1949 to 1952 multiple papers showed links between recent injections and patterns of individual paralysis cases during polio epidemics.2 If all the polio cases who had recently received a contemporary diphtheria or pertussis vaccine in the left arm were examined, for example, it would turn out that their left arms were paralyzed more often and more rapidly than the expected background rate. And generally, overall rates of paralysis would be quite high if one compared to statistically-collected controls.
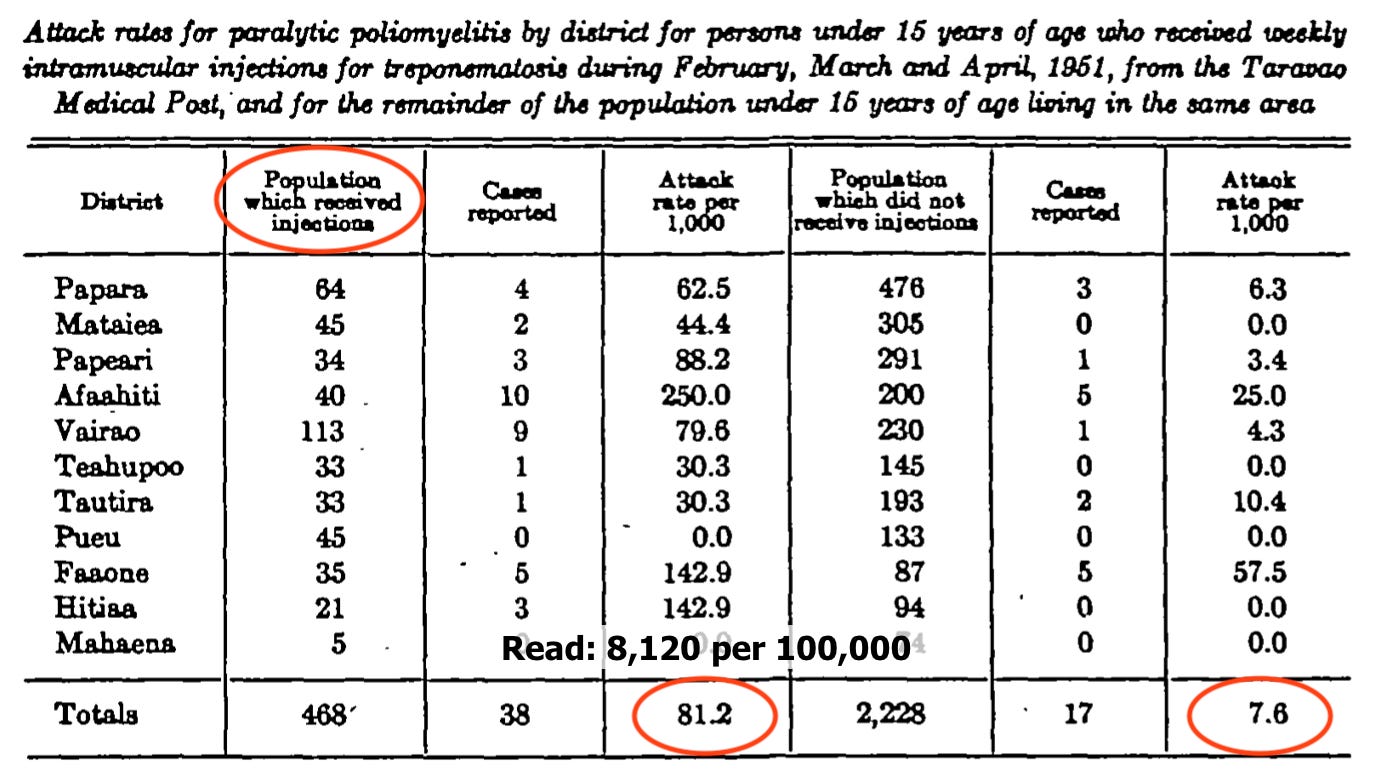
Rosen, L. Thooris, G. (1953)3
A single example suffices for the early studies, from the first known paralysis outbreak in French Polynesia, in 1951. Tahiti residents who had been actively receiving IM injections for treponematosis, including 468 youths, experienced paralytic polio at rates which were only exceeded a handful of times elsewhere.4 Neighboring children in the service area of the clinic were not so affected:
Strebel, et al. (1995)5
Numerous studies have continued to observe provocation polio into the modern era, typically in association with injections coincident to receipt of the oral polio vaccine. It is sufficient to briefly mention the case of Romania, where post-OPV polio rates were several times higher than other countries. Here, an association was found with recent injection of penicillin, implying a modest increase in overall polio incidence. (Romania culturally favored injection over oral medicine in general, and so penicillin continued to be injected long after oral forms became more common elsewhere. This is also why high rates of HIV infection were inflicted on orphans.6)
The incompatibility between the modest increase suggested by this statistical study, and the many-fold higher rates of overall polio in Romania, will be central to the argument in Pt. 2 that most polio epidemics are caused by injection-induced cases.
Not just vaccines, but all intramuscular injections
What is perhaps most significant about the Tahiti incident and the Romania study, and Bodian’s monkey study (below), is expansion of the type of injections found to cause increased paralysis beyond merely “vaccines” — in contrast to several of the human and mice studies already mentioned. This point will be brought up again when discussing the likely limitations of statistical studies into post-injection paralysis.
Tonsillectomies, too
It can be mentioned briefly that similar associations were found between a history of tonsillectomy of any duration, and increased rates of overall and especially bulbar paralysis (with the overall rate increase driven by the additional bulbar cases).7
Since normally tonsils (in chimp and monkey models at least) are the first sites of infection, we can tentatively assume that the “provoking” effect of removing them is similar in etiology to injections of unrelated substances which will be reviewed below — it is something related to injury or insult, rather than “exposure.”
Animal studies
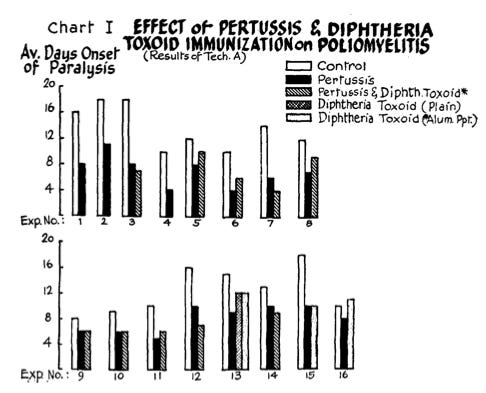
Milzer, et al. (1951) and Findlay and Howard (1950)8
Mice which receive unrelated vaccine injections become paralyzed more quickly after the Lansing polio strain is inoculated into their brains. Multiple experiments involving hundreds of mice often show that paralysis occurs twice as quickly.
Bodian (1954, 1955)9
Cynomolgus monkeys injected intravenously with polio virus (to crudely mimic human viremia) develop paralysis more frequently if they also receive unrelated and even inert intramuscular injections; paralysis more often occurs or develops first in the injected limb.
Bodian offers an argument for why the etiology for increased paralysis is not invasion of and via the peripheral muscle nerve; his reasons are not convincing and may be dismissed in light of later experiments.
Gromeier, M and Wimmer, E (1998)10
No further attention seems to be given to the experimental side of the question until 50 years after Bodian’s paper. This begins the modern era of research into the etiology of polio, which though limited, has sufficiently answered the biggest questions.
In an experiment involving transgenic mice who are artificially susceptible to human polioviruses, 3 saline injections were given intramuscularly after inoculation of polio into the tail vein. This is close to a mouse-model version of Bodian’s monkey experiment, except for the unfortunate problem that all mice tend to be paralyzed when inoculated in this fashion.
It was found that the unrelated saline injections caused more rapid onset of paralysis. Further, contradicting Bodian’s opinion, severing of the nerve from the site of the injections completely interrupted this provoking effect. This would appear to affirm that the etiology of “provocation” is a resulting infection of the nerves in the muscle during the viremia stage, and transit of polio virus into the spine from the same. (Of course, the unfortunate fact that all the mice become paralyzed in the end anyway prevents attaching certainty to this conclusion.)
Ren and Racaniello (1992) and Ohka, S. et al. (1998)11
Two other teams conducted similar experiments on severing the sciatic nerve in the early stage of polio infection in transgenic mice. This is not a “provocation” experiment in the true sense — polio virus was injected intramuscularly — but it refutes the objections raised by Bodian to the theory that provocation results from infection of peripheral muscle nerves.
In Ohka, et al., promptness of severing the sciatic nerve after IM-polio-inoculation corresponded directly to protecting mice from early paralysis.
Lancaster and Pfeiffer (2010) and Luethy, LN et al. (2016)12
Finally, a two more recent studies demonstrated the exclusive early enhancement of polio virus (and not two other viruses) after subsequent inert needle injection in a transgenic mouse model.
In this, polio was once again inoculated intramuscularly, which adds a redundant element as far as validating the “normal” mechanism of provocation. However, the results are still remarkable.
Injection — referred to by the authors as “muscle damage” — consisted of 5 insertions of a needle near the injection site at different times (some mice before polio inoculation, some after). Since mice were sacrificed at 24 hours, very little virus could be found in the brain of the immune-competent mice who were not given the subsequent needle injections. Levels of virus in the mice “damaged” by injections were “>270,000-fold higher.” This compares to an 8,000-fold increase found in uninjured, but immunocompromised mice vs the uninjured immune-competent mice. In other words, needle injection resulted in 30 times more increase in neural invasion than did immunocompromise.

In the earlier study by Lancaster and Pfeiffer (who is the final author listed in the 2016 study), a similar increase in retrograde axonal transit after unrelated needle injections was found for both polio virus and wheat germ, suggesting that needle injection removes normal barriers to fast axonal transit that would otherwise limit polio invasion. These are only two papers, but they suggest a more detailed mechanism for just how “provocation” takes place — by making transit of viruses more efficient in the sciatic nerve, thereby disabling a normal protective barrier between infected peripheral nerves and the spinal cord. It would be premature to consider this minute detail to be fully illuminated on the basis of such a small number of experiments, especially since they do not simulate viremia.
Most importantly, in the 2016 study, the “provoking” effect is only found for polio virus, not the other two neural-invasive viruses studied. In other words: polio virus is (as far as we know) uniquely “sensitive” to the enhancing effect of unrelated injections.
Summary
Post-injection polio “provocation” is a result either of increased susceptibility of peripheral nerves in muscles to invasion by polio virus during viremia, or improved shunting of virus from peripheral nerves to the spinal cord motor neuron stack.
With the (corrected) etiology established, we may now ask the question of whether needle injections in general were responsible for the great increase in epidemic paralysis in the 20th Century — a question science has failed to even ask.
Key to this question is one simple point: Injections make polio paralysis more likely upon subsequent infection, by promoting viral invasion of the central nervous system from peripheral nerves. How long after injection does this effect last?
If you derived value from this post, please drop a few coins in your fact-barista’s tip jar.
Paul, JR. “Historical and Geographical Aspects o G. “Poliomyelitis in French Oceania; epidemiologic observations on an outbreak with notes on the incidence of paralysis following intramuscular injections.” Am J Hyg. 1953 Mar;57(2):237-52. doi: 10.1093/oxfordjournals.aje.a119571.
The list is expansive; the major works are below and will be properly formatted later.
1950 burnet et al poliomyelitis following inoculations pub free
1950 Hill Knowelden Inoculation and Poliomyelitis pub free
1950 mccloskey poliomyelitis and immunization against whooping-cough and diphtheria pub free
1950 Martin Local Paralysis in Children after Injections pub free
1950 Martin Poliomyelitis in England and Wales 1947-50 pub free
1952 The Relation Between Recent Injections and Paralytic Poliomyelitis in Children pub free
Rosen, L. Thooris, G. “Poliomyelitis in French Oceania; epidemiologic observations on an outbreak with notes on the incidence of paralysis following intramuscular injections.” Am J Hyg. 1953 Mar;57(2):237-52. doi: 10.1093/oxfordjournals.aje.a119571.
Namely, in Nauru in 1910 and Chesterfield Inlet in 1949, which had similarly small populations — per the compilation of virgin soil outbreaks in
Sample, DW. Evans, CA. “Estimates of the infection rates for poliomyelitis virus in the years preceding the poliomyelitis epidemics of 1916 in New York and 1945 on Mauritius.” J Hyg (Lond). 1957 Jun; 55(2): 254–265.
Strebel, PM et al. “Intramuscular injections within 30 days of immunization with oral poliovirus vaccine--a risk factor for vaccine-associated paralytic poliomyelitis.” N Engl J Med. 1995 Feb 23;332(8):500-6.
Hersh, BS. et al. Risk factors for HIV infection among abandoned Romanian children. AIDS. 1993 Dec;7(12):1617-24. doi: 10.1097/00002030-199312000-00012.
Anderson 1954 Absence of tonsils as a factor in the development of bulbar poliomyelitis doi: 10.1001/jama.1954.03690310001001.
Weinstein 1954 A study of the relationship of the absence of tonsils to the incidence of bulbar poliomyelitis doi: 10.1016/s0022-3476(54)80086-2.
(Will be reformatted later.)
Milzer, A. Weiss, MA. Vanderboom, K. “Effect Of Pertussis, Diphtheria Toxoid And Salmonella Immunization On Experimental Poliomyelitis.” Proc Soc Exp Biol Med. 1951 Jul;77(3):485-8. doi: 10.3181/00379727-77-18823.
Findlay, GM. Howard, EM. “Nonspecific shock in experimental poliomyelitis.” J Pathol Bacteriol. 1950 Jul;62(3):371-82. doi: 10.1002/path.1700620309.
Bodian, D. “Viremia, Invasiveness, and the Influence of Injections.” Ann N Y Acad Sci. 1955 Sep 27;61(4):877-82.
Gromeier, M. Wimmer, E. “Mechanism of Injury-Provoked Poliomyelitis.” J Virol. 1998 Jun; 72(6): 5056–5060.
Ren, R. Racaniello, VR. “Poliovirus spreads from muscle to the central nervous system by neural pathways.” J Infect Dis. 1992 Oct;166(4):747-52. doi: 10.1093/infdis/166.4.747.
Ohka, S. Yang, WX. Terada, E. Iwasaki, K. Nomoto, A. “Retrograde transport of intact poliovirus through the axon via the fast transport system.” Virology. 1998 Oct 10;250(1):67-75.
Lancaster, KZ. Pfeiffer, JK. “Limited Trafficking of a Neurotropic Virus Through Inefficient Retrograde Axonal Transport and the Type I Interferon Response.” PLoS Pathog. 2010 Mar; 6(3): e1000791
Luethy, LN. et al. “Comparison of three neurotropic viruses reveals differences in viral dissemination to the central nervous system.” Virology. 2016 Jan; 487: 1–10.











Wow! Great article and very well researched. I guess it begs the question of whether there are agents (eg Vitamin D?) that are neuro protective against this effect. However it's not as likely to get funding if it's drawing attention to an uncomfortable truth...
Ok, so here’s a theory! Damage caused by tonsillectomy/ vaccine injection/ just trauma from a needle insertion causes either/or both
i) change to local microbiome so protection from polio is lost locally
ii) an immune response which attracts immune cells. If these cells just happened to be dealing with some polio then the polio gets taken to the site of injury and gets a head start on the nerve. Obviously eagerly awaiting next instalment to see what the time delay between the trauma and the increased risk of paralysis is and then need to know how long ‘healing’ an injury takes from an immune cell point of view.