Tolerance and severe disease, pt. 1
Just what, actually, *is* "Covid-19 pneumonia"? Interpreting the significance of IgG4 for future infections is helped by understanding severe disease to begin with.
Summary (click to expand):
Contents:
Part 1 (this post):
The myth of secondary bacterial pneumonia.
Sky-high rates of antibiotic use among hospitalized “Covid-19” patients.
The case for inflammation being (mostly) a bystander to Covid-19 pneumonia, not the cause.
The Myth of Cytokine Storm
Typically, “Severe Covid-19” is described and understood as an “immune over-response.”
A global conception of the disease resulting from speculative flu pandemic “research” and a handful of early papers from China further affixed the semi-mythical concept of “cytokine storm” to Covid-19, again emphasizing the role of response to the virus over the virus itself.
Based on these premature reports — and despite the fact that “cytokine storms” don’t even have a definition —
Cytokine storm has no definition.1
— Western doctors were primed to expect cytokine storms; Western researchers opined over and over and over that cytokine storm was a feature of Covid-19. The myth became a sort of reality of its own — a collective, three-year scientific daydream.
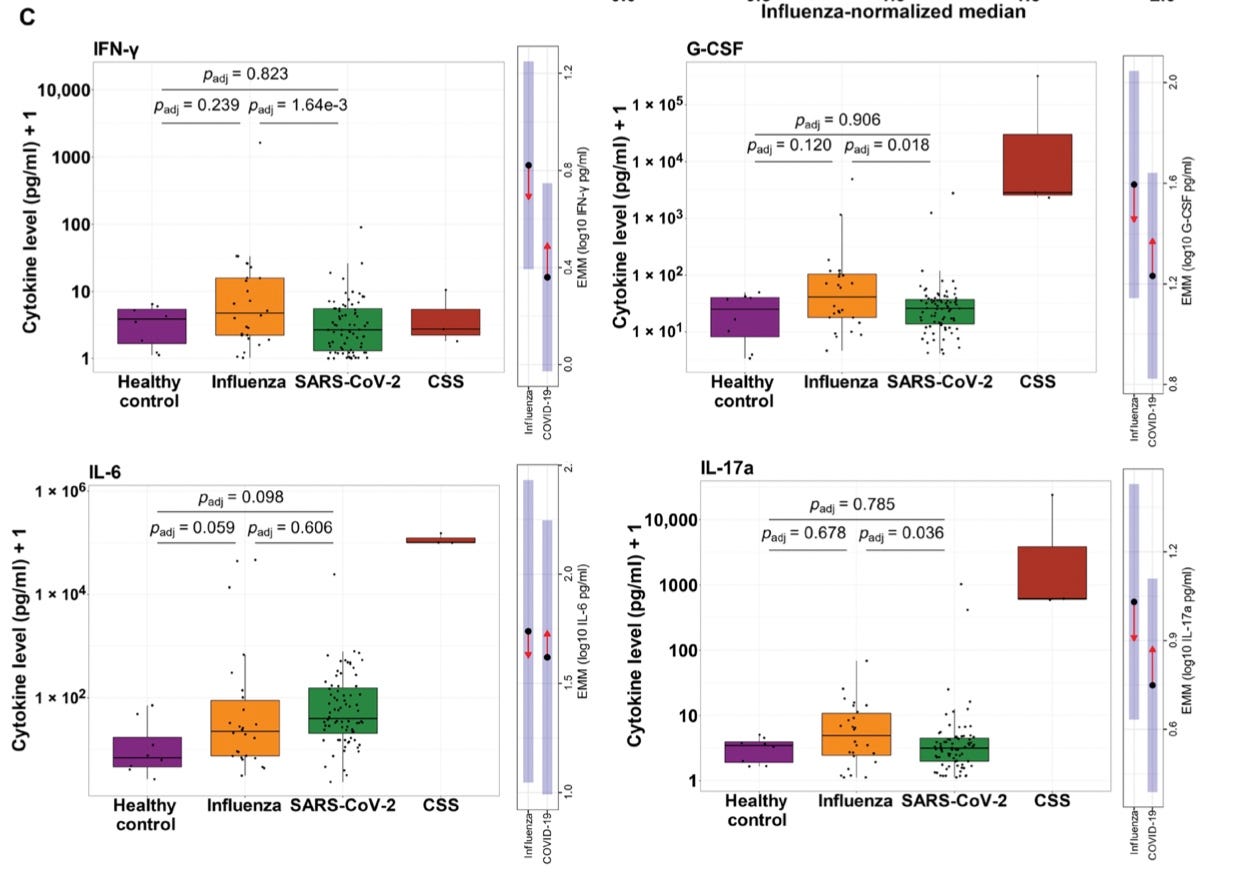
This despite the fact that the earliest papers did not in fact reveal anything impressive about the inflammatory and cytokine responses of hospitalized and ICU-admitted patients to begin with.

But the disease known as Covid-19 is not an “over-” response; and the cytokine storm is not a feature of it.
Authors Sinha, Matthay, and Calfee soundly rejected the term’s use in June of 2020:2
Is a “Cytokine Storm” Relevant to COVID-19?
Absent convincing data of their effectiveness in COVID-19, [anti-cytokine] drugs such as tocilizumab and sarilumab […] are being used to treat patients; trials of these agents typically cite the cytokine storm as their rationale […]
Enthusiasm for the use of immunomodulatory approaches in COVID-19 seems to derive in large part from clinical experience with cytokine release syndrome (CRS), a term frequently interchanged with cytokine storm. In the 2016 study of CRS by Maude and colleagues […] the peak plasma IL-6 level in patients who developed CRS was approximately 10 000 pg/mL—almost 1000-fold higher than that reported in severe COVID-19. […]
Although the term cytokine storm conjures up dramatic imagery and has captured the attention of the mainstream and scientific media, the current data do not support its use.
A month later, Remy, et al. wrote:3
Severe immunosuppression and not a cytokine storm characterizes COVID-19 infections.
The results from the present study strongly suggest that the primary endotype of COVID-19 is one of immunosuppression rather than hyperinflammation. Therefore, the approach of broadly inhibiting the host inflammatory response may be misguided, and may actually worsen clinical trajectories in some COVID-19 patients due to further impairment of an already compromised host protective immune response.
Circulating cytokines in COVID-19 patients, at least early in their clinical course, did not show widespread elevation. Most COVID-19 patients had either no elevation or only mild increases in the major proinflammatory cytokines including TNF-α, IL-1α, IL-1β, IFN-ɣ, etc
Finally, a related group of authors from the Washington University School of Medicine wrote in December:4
Distinct inflammatory profiles distinguish COVID-19 from influenza with limited contributions from cytokine storm
Multiple forms of COVID-19 immune dysregulation were observed: a cytokine storm phenotype in 3 to 4% of patients across primary and validation cohorts (7 of 168), a TH22 phenotype in 3% of the validation cohort patients (3 of 89), and a far more common phenotype characterized by targeted immunosuppression relative to influenza-infected patients. The signatures of this common COVID-19 phenotype compared to influenza were equivalent levels of IL-6 and IL-8, paired with lower levels of cytokines in many other pathways and essentially the absence of any type I or type II IFN response.
Mudd, et al.’s groundbreaking paper has a 6,000-odd access score at Science to date; compared to a mind-numbingly named pro-cytokine storm paper which scores at 33,616. Why can’t the message that Covid-19 is a disease of immune suppression, not immune overreaction, pierce through this great misunderstanding?
Is it because…
inhibiting the host inflammatory response may be misguided, and may actually worsen clinical trajectories5
Hm….
The over-response myth and IgG4
Based on these widespread conceptions, an early theory to explain the efficacy of Covid vaccines against severe disease, among those in the vaccine skeptic space who didn’t simply dismiss all the evidence of the same, was that these same injections were somehow tempering the “over-reaction” to the virus.6 And yet now, emerging IgG4 tolerance is largely predicted by vaccine skeptics to be bad (exactly as I said in July when first reviewing Irrgang, et al.7). Well, which is it?
Naturally, mainstream immunology is now pondering the same conundrum:8
You aren’t just imagining the poetic tone of the title. Pillai is a both a modern titan of immunology and a throwback to an age of rampant wordplay in biological education and publishing.9
Before we get to his comments on IgG4, we can conveniently use Pillai’s previous masterly talk on the disease Covid 19 itself to help set straight just what the disease is:
Pillai incredibly begins with a poem (that part of the sentence isn’t incredible, the next is) that functionally hosannahs the cytokine storm to high heaven:
An immune system that is balanced,
That generally is the norm.
But sometimes immunity goes berserk,
And the virus starts a storm.
He then introduces his talk as one that will illuminate how the over-response comes about. But a careful viewing in fact illuminates that there is no over-response per se; and cytokine storm is never mentioned. (By “careful,” I mean by noticing that Pillai leaves out any discussion of direct tissue destruction, only of the response to same, in order to substantiate his framing). I have thus reproduced the structure of his talk, but with comments on tissue destruction added.
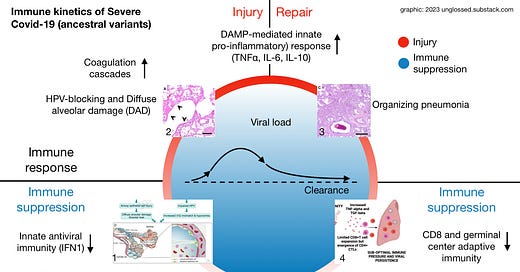
Severe Covid-19 explained: Immune suppression, massive tissue destruction, and injury response (leading to more immune suppression)
Overview:

Like all successful viruses, especially coronaviruses, SARS-CoV-2 is packed to the gills with innate immune suppressing weaponry — otherwise, viruses wouldn’t be able to infect any of our cells at all, given how many weapons we have in the other direction.
Pillai reviews some of the weapons the virus uses to evade immune detection once inside a cell, including blockage of our own RNA in our ribosomes; processing of its own RNA molecules to meet integrity checks and avoid destruction; and the creation of “replication factories” where viral RNA can be sequestered until the same processing occurs, after which it is exported by specialized pores. Ultimately, nearly 3/4 of the amino acids coded for by SARS-CoV-2’s genome are devoted exclusively to these intracellular structures and activities (and even the remaining 1/4 structural proteins, including spike, obviously partake in immune evasion as well).
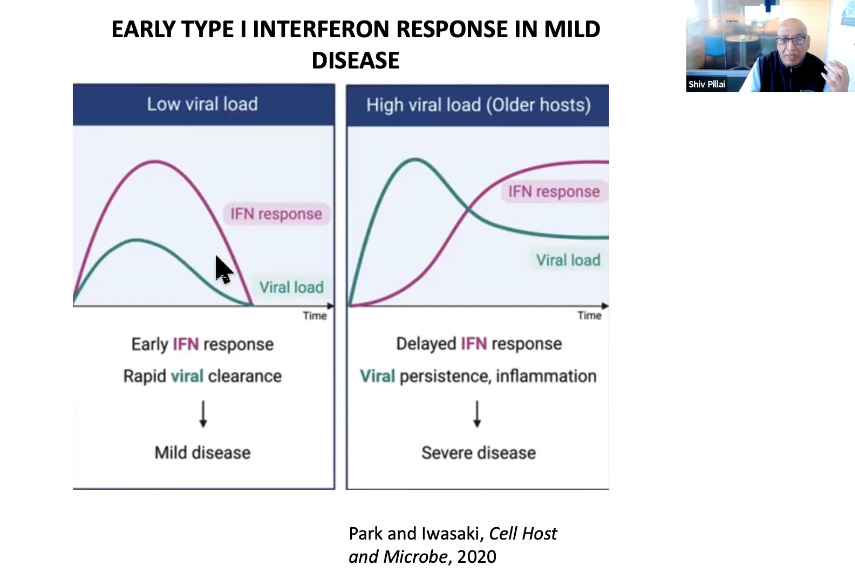
Individuals who experience milder or asymptomatic disease are those mount a successful antiviral response in cells adjacent to those which are infected and disabled by the virus. In severe infections, antiviral response, especially interferons (IFN), are functionally silenced. This leads to the paradox of severe secondary inflammation:
Pillai initially characterizes this inflammatory secondary response as immune attack. But what does he say is prompting the attack? Namely, and emphatically, “PAMPS” and “DAMPS” (19:50). PAMPS are molecular signatures of microbes — in this case SARS-CoV-2 — and DAMPS of tissue and cell death and destruction.
Just how much death and destruction is the immune system responding to, and can the response therefore be validly characterized as overkill? This is what Pillai fails to address, so let’s turn to some other works both recent and old.
Part 2 will discuss the real nature of lung destruction in Covid-19 — DAD and Organizing Pneumonia, in other words acute injury and injury response — and another myth (this one now popular on “our side”): that of a role for bacterial secondary infection in severe outcomes.
A note: Although the citations on this series will be narrow, it is the result of a few months of catching up with the evidence regarding the pathology of severe Covid-19, a topic I was formerly rather weak in.
If you derived value from this post, please drop a few coins in your fact-barista’s tip jar.
Sinha, P. Matthay, MA. Calfee, CS. “Is a “Cytokine Storm” Relevant to COVID-19?” JAMA Intern Med. 2020 Sep 1;180(9):1152-1154.
ibid.
Remy, KE. et al. “Severe immunosuppression and not a cytokine storm characterizes COVID-19 infections.” JCI Insight. 2020 Sep 3; 5(17): e140329.
Mudd, PA. et al. “Distinct inflammatory profiles distinguish COVID-19 from influenza with limited contributions from cytokine storm.” Sci Adv. 2020 Dec; 6(50): eabe3024.
(Remy, KE. et al.)
And so we have the question of whether cytokine storm was predictive programming. The term itself is essentially an anachronism — a niche symptomology observed in response to some treatments that was retroactively ascribed to SARS-1 and flu in the years after 2003. More history is at
Tisoncik, JR. et al. (2012.) “Into the Eye of the Cytokine Storm.” Microbiol Mol Biol Rev. 2012 Mar; 76(1): 16–32.
Note co-authorship of the Wellcome Trust’s Jeremy Farrar — this paper itself may be an element of the propaganda to pre-associated cytokine storms with the next pandemic, i.e. SARS-CoV-2.
Untangling the impact of the cytokine storm myth on treatment approaches, like quantifying the effect of suppression of therapeutics, remains difficult. But it may be one more thread on the tapestry of a widespread iatrogenic massacre.
Before calling IgG4 a “trainwreck of all trainwrecks,” for example, the blogger who goes by “Radagast” instead claimed that tolerance is good. This mirrors the uncertain response of mainstream immunology to the IgG4 news.
See “Tolerance Cometh.”
Pallai, S. “Is it bad, is it good, or is IgG4 just misunderstood?” Science Immunology. 7 Feb 2023.












My understanding of Covid-19 science is that we have little understanding of what "severe covid" is.
In a similar vein, we barely understand what "long Covid" is, argue over definitions, and avoid systematic look, allowing nonsense to proliferate, while a significant percentage of the population becomes effectively unable or unwilling to work.
So we are shooting in the dark here.
Do people have ground glass opacity and lung fibrosis because of overexpression of the virus, or immune overreaction, or both?
What exactly makes people more likely to have heart arrhythmia after Covid? What is the mechanism?
Nobody knows.
You are looking in the right direction, no doubt. However the answer may not yet be definitively known.
Such is the state of covid science, they are more interested in receiving grants than saving people.
You would hope that our govt would spent a billion or two on understanding "how Covid works", "how Covid spreads", and "what is long Covid" and "why are people dying suddenly at increased rates".
Nothing is happening and instead good substackers like you are trying to solve puzzles for which we may not even have the data necessary for a definitive answer.
Quote: "The myth became a sort of reality of its own — a collective, three-year scientific daydream."
AFAIK, autism does not have a definition, yet it is real. That is, legally it is the psychiatrist the one expert who gets to label a child as autistic. His opinion is "science." But everyone knows that there has to be some damage to the brain or other organs that is characteristic of what we call autism. That should be the objective definition. But there is no objective definition, yet. Am I wrong on this?
This situation creates funny decades-long daydreams, which leads to people getting the label of High-functioning Asperger Syndrome. Which is a complicated way to say someone is weird, like myself.
I didn't get that label when I was told to go get that label for yourself. That was because the psychiatrist (male, mid 40s) who saw me back then was clearly on his way out of all the psychiatric pseudoscience. He was let down, and didn't want to augment the mountain of false diagnoses with one more little grain. That's what it looked to me he was doing. He looked very tired of everything in his specialty. I wouldn't say depressed, much rather, he became realistic.
I wasted time being scared from these wild claims such as "cytokine storm" and "ferrets dying from antibody-dependent disease enhancement" and other things that have been thrown to members of the public for many years, long before the internet, to abuse them and create a profitable state of general hysteria. I'm sorry I collaborated with that by not being a good critical thinker.
Now I'm learning. I don't want to be weaponized again, if I can avoid that. I wish other people would try to learn too.