A topical Friday post arrives again. On the docket:
Thursday’s “Breakthrough” Lower-Transmission(?) Study!
Here in the 21st Century if you don’t like the truth, just wait five minutes.
A recurring motif of the Pandemic™ has been the amplification of the rapid upturning of prior scientific consensus, and subsequent reversal of the upturning, which so distinctly characterized the TV news “studies say” coverage of the last quarter-century. In fact, I have a sweeping essay reflecting, in part, on the manner in which “studies say” coverage seemingly primed us for the current grand experiment in panic-spreading and manipulation. This has been in draft for over two months; I’m waiting until I finally decipher in what way that priming could have been weaponized, before finishing it.
The very nature of Covid Revisionism, after all, has been that media-reported study results have undermined the narrative nearly as often as they have supported it - as if The Science has been playing a game of chess with itself, ineptly advancing pieces on both sides of the board. It is only in the wake of the summer’s sudden and final clearing of so many of the narrative battlegrounds - natural immunity, masking and Covid vaccine efficacy - that the continued perpetuation of revisionism appears deliberate and one-sided.
Here, I do not speak of new research which provides a signal that these cleared battlegrounds may in fact be under dispute, perhaps because of an evolution of conditions on the ground. I would not find such a signal troubling - because to do so, would be to fall into the “settled science” trap. It’s entirely possible, even likely, that some elements of the current understanding of the virus and the pseudo-vaccines will be reversed - that does not mean it is unreasonable to proceed for now as if they won’t be. Action is only ever possible in accordance with whatever abstract, but flawed mental image of reality prevails at a given moment.
Instead, I speak of the sudden, concerted arrival of outdated research which apparently seeks to upturn the advances in our consensus understanding during the summer.
I have no wish to spend the coming autumn playing whack-a-mole with studies from last winter and spring that the media tease as a “vindication” of the failing Covid vaccines, particularly as it is quite difficult to do so without winding up in a defensive intellectual posture, which leads to self-reinforcing errors. Yet what choice do the first two of these studies give me?
June Gloom
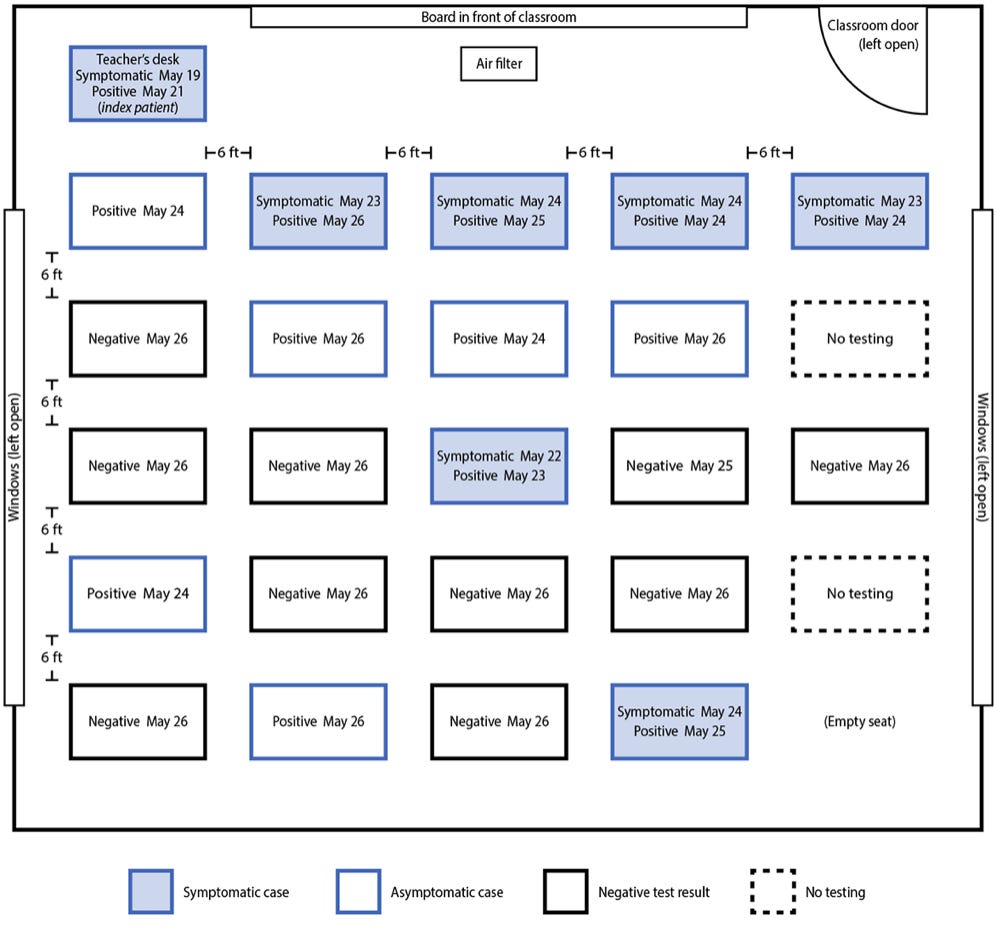
The CDC’s recently released study, “Outbreak […] in an Elementary School — Marin County, California, May–June 2021,” will surely be of great interest to parents who plan on time-traveling to late spring.2 Such parents will have a valid reason to contemplate a policy discriminating against unvaccinated teachers, on the grounds that their children may be exposed to SARS-CoV-2 in a school setting which would otherwise conceivably carry a lower risk of exposure.
Hopefully, such time-traveling parents would still conclude that since their children will eventually encounter SARS-CoV-2 somewhere outside of school anyway, especially over the summer when Covid vaccine infection and transmission efficacy evaporate, discriminating against such teachers would provide no net benefit to their children - to do so might make their child’s school year a little less bumpy, but that smooth school year might be followed by a disrupted summer in return.
For parents who are not time-traveling, of course, the Marin study is useless. Covid vaccinated teachers are just as likely to provide the virus with the infection bandwidth it needs for the coming winter wave as unvaccinated teachers are. Discriminating against unvaccinated staff and parents in a school setting does not make schools in any degree “safer.”
In the eyes of an epidemiologist, of course, evaluating the “net impact” of an outbreak totally misses the point: It is their job to obsess over the dynamics of viral spread within a population that has artificially attempted to suppress a virus, under the logic that such an obsession will enable humanity to achieve the eradication of respiratory viruses that the experts keep pinkie-swearing not to actually believe is possible.3 In this framework, vaccinating most of a population and daring a virus to achieve antibody escape for four straight months is merely the prelude to beautiful demonstrations of their mathematical wizardry:
Where’s the fun in mass experimenting on the entire human race, after all, if you don’t get to make any charts!
But nothing about such insular exercises in statistical wizardry and chart-making renders the mass experiment scientific. The teacher of the classroom where an outbreak occurred at this school was one of only two teachers who were unvaccinated, outliers among the remaining 22 Covid-vaccinated staff (only six of whom appear to be other teachers); that doesn’t tell us anything about what happened in every school in the country. And the teacher took off her mask to read: But that doesn’t tell us what would have happened if she hadn’t done so.
The students, meanwhile, were only PCR-screened for infection with SARS-CoV-2 starting four days after the unvaccinated teacher conducted class while experiencing “nasal congestion and fatigue” on May 19 - there’s no telling if the outbreak was not in fact seeded by one of the four asymptomatic test-confirmed positive (and pointlessly masked, 6-ft separated) students at the front of the class to begin with, who may have been infected well in advance of May 19, given that PCR-testing can produce a positive up to 90 days post-infection:4
However, let’s still acknowledge it as likely that the teacher played a role in amplifying the outbreak within the classroom, even if it was seeded by a student, and thus amplified the subsequent scale of secondary spread to siblings and parents as well. This can be argued based on the concurrently identified cases in other classes - four or five of which were in isolation (the study text is inconsistent), and six of which occurred in the class three grades higher and were partially cross-connected to a sleepover, resulting in only one confirmed parent infection. But with this likelihood acknowledged, there is still no way for the study to demonstrate that the teacher’s vaccination status or brief mask-lessness were instrumental to her amplification of the outbreak. It could merely be a question of where the (potential) actual original patient zero student was sitting in her class - such as in the front, as suggested above - compared to the classes with smaller outbreaks.
After all, it’s not like unvaccinated teachers are expected to prevent transmission of SARS-CoV-2 to begin with. The question is whether this study demonstrates that “if only X (vaccination or strict masking),” that expectation in fact should have prevailed. It does not. In fact, it offers significant collateral findings which should lead us to believe otherwise!
Despite constant masking and an absurd, patently superstitious desk-distancing scheme inflicted by their adult “caretakers,” the students in this and other classes were conferred little to no protection against classroom-acquired infection, providing clear evidence (as if any was needed) supporting the supposition that masks are powerless against a flood of .1µm particles saturating the air. What’s more, of the four parents who went on to develop symptomatic infection after in-home exposure to infected students, three were vaccinated.
four parents of students with cases were also infected […] Among the five infected adults, one parent and the teacher were unvaccinated; the others were fully vaccinated. The vaccinated adults and one unvaccinated adult [and the unvaccinated teacher] were symptomatic with fever, chills, cough, headache, and loss of smell. No other school staff members reported becoming ill. No persons infected in this outbreak were hospitalized.
This accords both with the likely high rate of vaccination in Marin, and the timing of the study - at the end of May, just when vaccine infection efficacy was beginning to wane.
The media has been enthusiastic in its trotting of the woefully-timed Marin study, which not only observes a reality that no longer prevails, but delivers those observations just as parents and school administrators are engaged in war over barbaric, outdated, and futile prevention policies. But if there’s one piece of advice to be crafted from this study, it is in fact to stop psychologically torturing children with pointless distancing and masks.
Meanwhile, whether the “Covid vaccine golden age” of the spring can even be recaptured with the rollout of (synchronized?) boosters has yet to be proven; and this study alone does not even demonstrate that in-school outbreaks would be prevented in any great number by such an endeavor.
Swab the Decks
The other outdated retrospective only appeared online yesterday. I have yet to see it make the media rounds; perhaps the news is resting its Trotting Elbow with warm towels at the moment. The study’s observations are neatly contained within its title: “Longitudinal analysis of SARS-CoV-2 vaccine breakthrough infections reveal limited infectious virus shedding and restricted tissue distribution.”6
Here, we may be very brief. Although the paper would seem to upturn the findings from July of high “virus-y-ness” among post-vaccination “breakthrough” infections (I continue to scare-quote the term, as there is no longer any protection to break through), it does not do so at all: Observed infection outcomes are among vaccine recipients who were only between 16 and 52 days post second-dose (as well as individuals who have not yet crossed the 14-day “fully vaccinated” threshold).
Thus, it says nothing at all about the likely transmission rates among individuals who are infected with SARS-CoV-2 more than six months post-vaccination!
In examining the CDC’s declaration that Covid-vaccinated individuals are likely to spread SARS-CoV-2 as easily as the unvaccinated, I was ambivalent about using the Barnstable County study as the basis for this conclusion.7 That study, like the “Breakthrough Infections” paper, uses PCR cycle-rates as a proxy for likelihood of passing the virus on: The more quickly a PCR test returns a positive, the more original material was present in the given sample. But does that really mean “more infectivity?” Comparing how much gasoline two cars have in their tanks at a given moment does not tell you how much driving they’ve done in the last week. Here I default to a presumption that immunity and infection are at least a bit more complicated than a swab can ever portray; especially since so much of the battle is always conducted far beyond the reaches of human vision. I thus argued, instead, that the best evidence for high rates of transmission among the Covid-vaccinated had already arrived, in the form of the Israel and UK delta waves. I still maintain this to be the case.
This study is nonetheless interesting in another respect, which is the use of oral swabs (represented by the light blue squares) as one of the markers of “infection.” In fact, one of the subjects - who was 52 days post- second dose - never would have been detected on a normal (nasal) PCR test to begin with. An earlier paper by the same authors includes additional interesting findings, along similar lines, but for natural infection: The virus is detectable in the mouth before the nose (I haven’t yet reviewed the earlier paper itself). There appears to be a second realm of transitional, asymptomatic “infection” with this and probably other respiratory viruses, yet to be well-explored. Overall, it makes for an interesting read, even if its conclusion - “Altogether, this study provides a set of high resolution data that ratify the role of the current SARS-CoV-2 vaccines” - is completely refuted by present-day reality.
“Saving Lives” with Social Decay
(For correction notice on this section, see footnotes.9)
I don’t care if masks work. I don’t care if they work directly. I don’t care if they work indirectly. I don’t care if they work inside but not outside; I don’t care if they work on young people or old people; I don’t care if they work on dead people! I don’t even care if they are strangling me with CO2 and promoting a fungal infection that will literally eat my brain! All I care about is that they’re stupid, and uncomfortable, and I’m not a baby, I’m a pig-headed American male who remembers what driving without a phone was like and I take that legacy seriously - and, most importantly of all, masks coddle one’s fellow human beings into being afraid of something they otherwise would learn to stop fearing, contributing to an endless plague of immune-suppressing anxiety and phobia.
Humans, it may astonish the average modern news-consumer to discover, have immune systems. They are built-in to our bodies. They do not need to be hermetically sealed off from the rest of the species; in fact we’re all more at risk from the immune system’s internal menu of hazard - cancer, autoimmune disorder - than the collective menu of hazard - viruses - anyway, so why would attempting to “shield” the immune system from the less risky menu do anything but plausibly lead to incompetence in dealing with the more difficult challenge?!10
So, while I will stand by my assertions that masks are useless at preventing the spread of a respiratory virus of any type on a community level and are plausibly detrimental to immune competence, I hesitate to actually defend these positions. I feel that to do so misses the point - a point which itself is better expressed by a middle finger thrust in the face of the fear of death, accompanied by downing a glass of rum and poison-laden Diet Coke.
Still, I feel I can meet this topic halfway when it comes to the controversial, recently released super-study, “The Impact of Community Masking on COVID-19: A Cluster-Randomized Trial in Bangladesh.”11 Here, I feel it is possible to litigate mask efficacy without ceding any ground on the larger principle.
The study’s methods are too grandiose to be adequately summarized - one is better off referring to the text itself, which is well-written, but cringe-inducingly authoritarian in outlook, and lamentably statistical. Suffice it to say I saw nothing wrong with the authors’ study design, aside from a staggering deficiency of faith in human free will and independent judgement. I think the authors did a good job in their attempt to “pair” intervention and control villages, and while some elements of their intervention program may have introduced bias, these were not used in all intervention locations. While the list of citations used to justify the particular design of their “mask promotion psy-op” convey a degree of hopeless alienation from the human race on the part of the authors that is embarrassing to behold, at least they were thorough in testing several of their intervention designs in the months preceding the trial period itself, which did not get rolling until mid-November and finished in early March (8 weeks after the first week of January).12
Our intervention was designed to last 8 weeks in each village. The intervention started in different villages at different times, rolling out over a 6-week period in 7 waves. There were between 14 and 59 village-pairs grouped in each wave based on geographic proximity and paired control and treatment villages were always included in the same wave. The first wave was rolled out on 17-18 November 2020 and the last wave was rolled out on 5-6 January 2021. […]
At 5 and 9 weeks follow-up, we surveyed all reachable participants about COVID-related symptoms. Blood samples collected at 10-12 weeks of follow-up for symptomatic individuals were analyzed for SARS-CoV-2 IgG antibodies.
The study results, on the other hand, are very difficult to critique, as very little raw data is provided - everything which comprises the sparse supplemental materials consists of various forms of statistical abstraction. The lay reader must therefor take the authors at their word:
The intervention increased proper mask-wearing from 13.3% in control villages […] to 42.3% in treatment villages […] Physical distancing increased from 24.1% in control villages to 29.2% in treatment villages. […] The proportion of individuals with COVID-like symptoms was 7.62% (N=13,273) in the intervention arm and 8.62% (N=13,893) in the control arm [and follow-up antibody testing observed a similar relative difference in rates].
And, that’s basically the whole thing.
Antibody testing appears to have been an afterthought in the study design, and is the weakest part of the results. The authors seemingly intended to “help show” what they take as a gospel truth - that increased masking would “save lives” - without initially designing any way to measure clinical outcomes. The study was thus not well-designed to demonstrate that masks actually “work” at all - only which methods of mask promotion led to greater partial adoption (of what was already legally mandated in Bangladesh, despite the widespread and universally unpenalized flaunting of the law).
But at some point when the trial was already underway, it apparently occurred to them that merely comparing survey-reported symptom rates was not even evidence of a meaningful impact on SARS-CoV-2 specifically. And because of the rushed antibody testing of survey-identified “positives” which resulted - blood was drawn within a few days of the end of the trial period - many of these positives would not yet have had time to complete “seroconversion” (the arrival, in the blood, of longer-lasting IgG antibodies).13 Thus, the rates of test-confirmed seropositivity per population obtained by the authors are abysmal: The authors report 0.68% positivity for intervention villages and 0.76% for control villages. But because antibody tests were only directed toward individuals who self-reported symptoms in the trial surveys, with roughly equal rates of survey “positives” consenting to provide a sample, the seropositivity rate at least partially recycles the survey rate: More samples were collected for the control group, and thus more positive antibody tests were captured relative to the population as a whole.14
And regarding the potential that the third-party “observers,” able to decipher which villages were “treatment” and control, systematically fudged their results to make the researchers feel better - well, sure, it’s a possibility. I will represent this possibility as 50/50, since I am no expert on the psychology of that most mysterious of beings, the Bangladeshi village-masking-observer-for-hire. Biological and medical research would be better off in general if it made a firm commitment to data chain of custody - but what do I know, I never made it my business to sell drugs based on second-hand efficacy data.
So.
If the study’s results are accurate - a shaky conclusion at best - would that mean the increased masking marginally slowed spread during the trial period because little strips of porous cloth somehow repelled microscopic airborne particles - or because being hectored by the intervention program made villagers more wary of each other, as reflected by the increase in social distancing? And would the latter mechanism translate to other countries, with completely different economies?
Who cares, because Bangladesh was not even experiencing a wave during the study period.
Any questions of “non-medical intervention” efficacy need to be both held up to and critiqued according to the novel model that preventing the health care system from being “overwhelmed” is worth the demonstrable and innumerable, potentially lifelong ills that come from forcing a social organism to pretend to be an automaton for months on end.
The Bangladesh study does nothing to accomplish the former and faces severe challenges from the latter, because it does not demonstrate the following:
Intervention villages did not go on to have higher rates of infection in the remaining period before the spring wave.
Intervention villages did not go on to have higher rates of infection during the spring wave.
Hypothetical intervention villages with higher masking during the spring and summer waves would also have demonstrated reduced spread.
Hypothetical intervention villages with higher masking during the spring wave, if they did demonstrate reduced spread, would not have gone on to have higher rates of infection during the summer wave, with the result that health care systems would be more overwhelmed than they would have been in the absence of the intervention.
Repeat X infinity.
This is just intuitive: slowing spread in the short term does not mean reducing it in the long term nor even not speeding it up it in the future short term.
The Bangladesh study is as useful as observing that children who do not pick up their toys every day spend less time with the toy chest open over a two day period. They will obviously catch up for that debt, if not pay a premium, eventually. The villages in the study likewise have no way to avoid paying for any immune debt that they create in the trough between waves.
What are they supposed to do? Hold out for a year or two until they receive a rushed, experimental vaccine that might turn out to enhance infection a year or two later? That seems like something only a lunatic would come up with!
So of course this error in thinking has been entirely affirmed in the lunatic mainstream press’s reception to the study, as epitomized by The Asylum article arriving after the original edition of this post, “The Masks Were Working All Along.”15 The article takes the Bangladesh study to affirm that our “excellent” flimsy, fear-inducing masks have been “definitively” working (eh) - OK, working to do what? Pointlessly push cases backward in time so that this year’s waves were higher? While all the while destroying waterways and stunting or reversing the psychological development of the entire human race? It’s certainly possible - this study only expresses the first part of a demonstration of such a mechanic. But “Who cares?!” the acolytes of public self flagellation would likely reply to these questions.
Indeed. Who cares.
There is a term for the way we have been thinking about preventing the spread of SARS-CoV-2 from the start: Short-sighted.
One of the most significant consequences of the destruction of the Herd Immunity Myth is that we no longer have any justification for doing so; but since herd immunity was foreseeably a myth from the very beginning, we never did.
And now, off to my CDC-counterindicated vaxx-free Labor Day beach weekend!
Lam-Hine, Tracy. et al. “Outbreak Associated with SARS-CoV-2 B.1.617.2 (Delta) Variant in an Elementary School — Marin County, California, May–June 2021.” cdc.gov
“Asymptomatic spread controversy disclaimer.” / For duration of positive testing after infection, citation pending.
(index link anchor)
(index link anchor)
Corrections have been made to this segment, which all reflect that my initial analysis of the study was too generous in several respects:
1. The initial version of this post incorrectly claimed that the intervention wrapped up in the first week of January, 2021. Roll-out of the intervention among grouped villages concluded in January. The intervention itself ended 8 weeks after roll-out for each group.
This only magnifies the critical flaw of the study as argued by this post, as case-rates were much lower in mid-January to early March than the were at the end of 2020:
Coincidentally, the authors quote a random seroprevalence survey conducted between October, 2020 and February, 2021 which found positivity rates for antibodies for SARS-CoV-2 of 71% in Dhaka (8,906,039 pop. in 2011) and 55% in Chattogram (2,592,439 pop. in 2011), leading to 68% overall. This suggests that the summer, 2020 wave was orders of magnitude larger than suggested by the graph, due to low testing.
The questions remain: Was rural Bangladesh on the same schedule as the cities during the summer 2020, or did SAR-CoV-2 largely not spread until spring 2021; what were the actual seropositivity rates for rural Bangladesh in general and these villages specifically heading into the study period and afterward; did rural Bangladesh partake in either or both of the spring and summer waves or were these still predominately cases recorded in Dhaka, Chattogram, or the “medium” sized cities (there are no other cities with over a million population in Bangladesh; excluding the top two cities, the population of Bangladesh is still virtually entirely rural; however, the limited prevalence of testing implies that the tiny sliver of population in medium sized cities could still dominate the recorded case counts).
But that the villages under observation were experiencing a wave at any point during the trial period, seems quite implausible.
2. Additionally, the original post repeated a claim encountered online that the author’s blood samples were “still being processed.” This is not the case; all valid samples have already completed testing:
We tested 9,977 (91.1%) of the collected blood samples [which comprised ~40% of the survey-identified “positive” individuals in both intervention and control villages] to determine seroprevalence for SARS-CoV-2 IgG antibodies. Untested blood either lacked sufficient quantity for our test or could not be matched to individuals from our sample because of a barcode scanning error.
Thus the following text was removed from my analysis: “I’m inclined to give the study a provisional pass on this point - particularly as the authors are, apparently, still processing additional samples, and a later update will either affirm or dispute the current result. “
3. Lastly, the original characterization of the seropositivity data as “affirming” the symptom survey results was seemingly rendered inaccurate by further review of the study text. I have edited the relevant text and added footnote 14 for further discussion.
In light of all these updates, the qualifier “a shaky conclusion at best” was added to the sentence beginning “If the study results are accurate…”
This alludes to my version of Immune Equilibrium theory.
Abaluck, Jason. et al. “The Impact of Community Masking on COVID-19: A Cluster-Randomized Trial in Bangladesh.” poverty-action.org
The study text claims that observation was between November and May. However, this does not match the indicated 8-week intervention schedule. It appears that observations after the 8 week intervention schedule were merely to investigate duration of mask adoption, but not incidence of survey-reported symptoms.
The 10-week observation was conducted two weeks after all intervention activities had ceased. We also collected longer-term data on mask-wearing behavior 20-27 weeks after the launch of interventions. […]
The owner of the household’s primary phone completed surveys by phone or in-person at weeks 5 and 9 after the start of the intervention. They were asked to report symp- toms experienced by any household member that occurred in the previous week and over the pre- vious month. […]
We collected capillary blood samples from participants who reported COVID-like symptoms during the study period. For the purposes of blood collection, endline was defined as 10-12 weeks from the start of the intervention.
The author’s used IgG-specific antibody assays, thus all but ruling out positive tests for many individuals still undergoing seroconversion.
Blood samples were tested for the presence of IgG antibodies against SARS-CoV-2 using the SCoV-2 DetectTM IgG ELISA kit (InBios, Seattle, Washington).
Notably, the authors’ text is quite jumbled and self-contradicting on the subject of how they calculated seropositivity rates, and absolute numbers of samples are not provided. The conclusion that more samples were collected for the control group is however robustly supported by the layout of sample return rates:
This amounts, as far as I can tell, to 128 additional samples for the control group. Using the survey-reported “positive” counts provided in the text:
(13893 x .399) - (13273 x .408) = 128
There are several ways to reverse-engineer the control group seroprevalence with this weighting removed; the simplest being to simply attack the reported percentage with a (control samples - 128)/(control samples) multiplier, which avoids having to account for the samples that were thrown out (pinning our hopes on the resulting ratio being similar):
Reported intervention group seropositivity rate
.0068
Reported control group seropositivity rate
.0076
Adjusted control group seropositivity rate
.0076 x ((13273 x .408)-128) / (13273 x .408)) = .0074
This is a small adjustment, but represents one fourth of the “prevented” positive results. This yields a value for deceptive “relative risk reduction” that is lower than the authors’ given “adjusted” value of “9.3%”:
((.0074-.0068) / .0074) x 100% = 8.1%
But with so much raw data hidden from view, these figures are no less shaky than the study’s own conclusions.
It is also unclear from the study text whether any seropositivity sampling was conducted before the trial period. In fact nothing at all in the main text supports such a conclusion; and yet the authors still apparently used something to calculate “baseline symptomatic seroprevalence” in their statistical analysis. My best guess is that “baseline” actually refers to seroprevalence among sampled individuals who were survey-identified as positive in the first week; which is not a baseline at all.
It is on this point that I feel there are strong grounds to dismiss the most narrowly-supported but “dramatic” and loudly-touted of results - the higher “prevention” signals in trial villages where surgical masks were used, particularly among the elderly:
In villages randomized to surgical masks (n = 200), the relative reduction was 11.2% overall (aPR = 0.89 [0.78, 1.00]) and 34.7% among individuals 60+ (aPR = 0.65 [0.46, 0.85]).
Do we really know if this corrects for different starting points? “Individuals 60+” seem to account for less than 10% of the population of Bangladesh. The large size of the study design cannot offer the same statistical protection to a fractional cohort as it does to the overall set, and the surgical mask trial elderly are a double fraction.
But even setting that aside, it is once again left in the open whether this dubious signal is the product of a disproportionate increase in indirect effects: Namely, that the elderly were more influenced by the intervention in terms of avoiding social contact, and that surgical masks for whatever reason heightened this psychological response. The “social distancing” difference recorded by observers, for example, did not account for the age of who was “distancing.”
Thompson, D. “The Masks Were Working All Along.” (2021, September 4.) The Atlantic. The author, who per bio opines to his bewildered Asylum audience about economics, technology, and the media (himself?), and hosts a podcast designated “Crazy/Genius” (I’ll hold off on believing he’s got the second part down), wrote quite a bit about masks during the spring, his last article appearing in May and conspicuously headlined “The Texas Mask Mystery - When the governor lifted the state’s mandate, liberals predicted disaster. But it never came. Why?” Apparently, in the mind of Thompson, who now takes an older study from literal Bangladesh to represent the erasure of formerly dispiriting evidence from close at hand, the answer is some form of cosmic test of faith in ludicrous and humiliating facial accessories.
/Substack tracking scrambler link (?): Fuel Performance adjustable dumbbells (walmart.com)/