The Virus Shuts Down Kids' Lungs Study
Frankly stunning rates of post-infection impaired lung function in a small study. But is it all a reflection of a hidden bias?
A new study provides strong apparent evidence that SARS-CoV-2 is above-and-beyond a normal virus in circulatory destruction — even in children.
However, the results are so dire that they suggest a hidden bias for rarer cases with more observed post-infection lung dysfunction (all cases are described as “mild,” none involved pneumonia or hospitalization).
Some subjects were Covid-vaccinated after infection; but corresponding lung function results are not indicated.
The study:1
The Set-Up
Children 5 - 18 were recruited from August to December, 2021 based on prior case criteria:
“Recovered”: Previous PCR+. Not reporting symptoms more than 4 weeks after the acute phase. N = 29.
This group had a similar age spread and mean weight as the control group.
All but 1 were Nucleocapsid-antibody seropositive.
1 was Covid-vaccinated before infection, 7 after.
“Long Covid”: Previous PCR+ and symptoms reported more than 4 weeks after acute phase. N = 25.
This group was a bit older and higher-weight than the control.
All but 3 were Nucleocapsid-antibody seropositive.
0 were Covid-vaccinated before infection; 11 after.
Both groups were 100% rated as “mild” for the acute infection; 0 were hospitalized.
Healthy control: Not previously PCR+, negative for antibodies to either Spike or Nucleocapsid. N = 9.
0 were Covid-vaccinated. (4 were excluded for being Covid-vaccinated.)

(There were a handful of pre-existing conditions in the infected groups (Table E1); nothing close to enough to drive the high numbers of subjects showing sub-normal lung function. Likewise, if post-infection Covid vaccination has any effect on lung function, it still cannot account for the numbers; and the signal for any influence in the “Long” vs “Recovered” rates and the time-from-infection rates is equivocal.2)
Subjects underwent low-field MRI, which measures morphology (structure), ventilation (air-flow), and perfusion (blood-flow). It is a non-invasive procedure; the authors seemingly did not expect findings alarming enough to warrant additional, more invasive tests which could have shed more light on what is going on in these kids’ lungs.
Scans were evaluated by a blinded technician, who did not know the infection / control status of any subject.
Fig. 2 demonstrates how air-flow and blood-flow are measured. The MRI finds where airflow is going and where blood-flow is going, and maps areas with both as green, areas with neither as purple, and areas deficient in just one as red or blue.
So the example “Long Covid” subject’s scan, because there is so much black in the airflow and blood-flow scans, has a ton of red and purple, and a lot of blue as well:
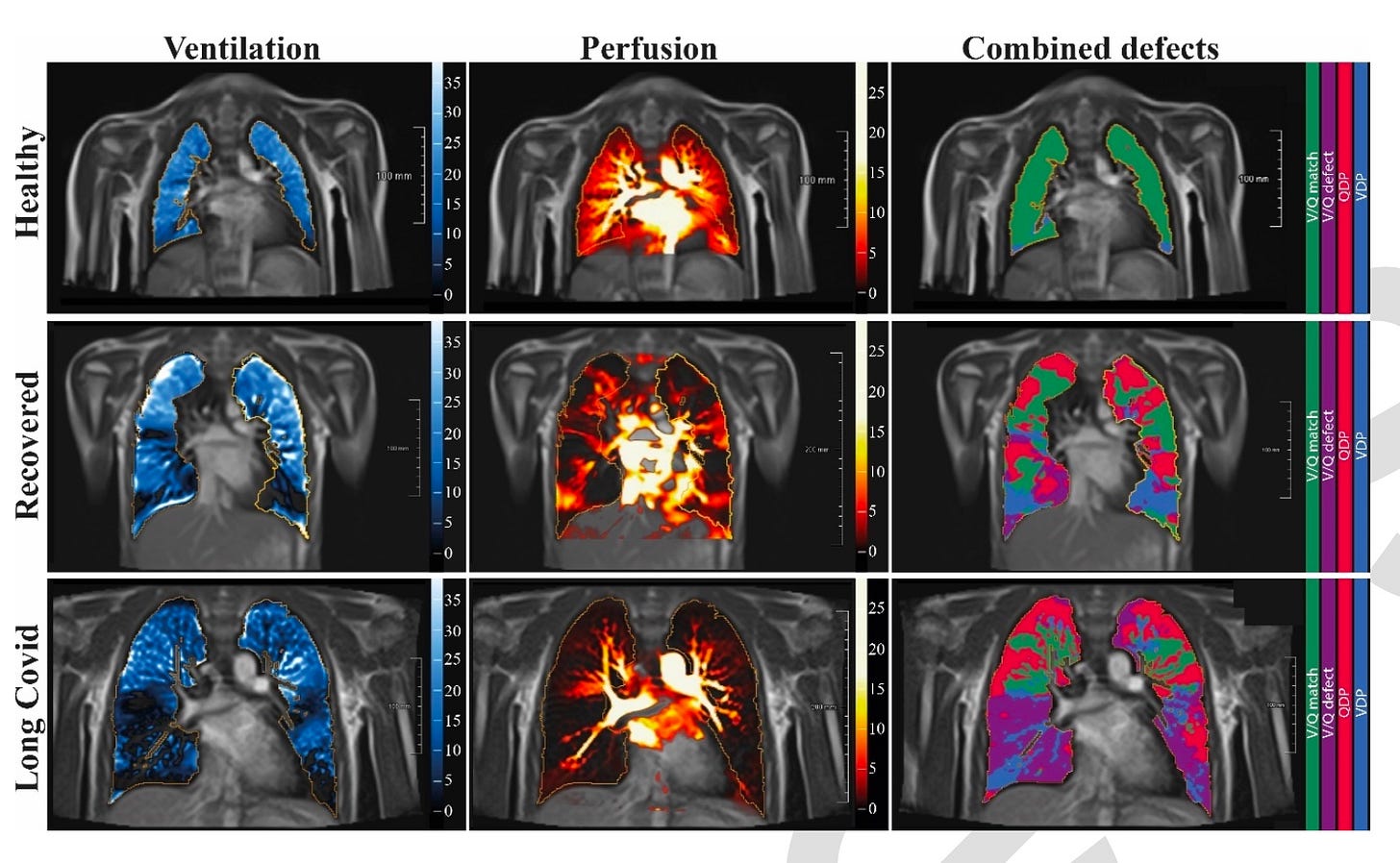
Because air has a harder time reaching the lower lung, it is common to have blue at the bottom. Likewise, because blood in the pulmonary circuit is sensitive to gravity, it is common to have red at the top. Elsewhere, there should be both (green, usually low 80% of the lungs); and nowhere should be neither (purple). But naturally, only green areas can perform the job of getting oxygen into the blood (and CO2 out), as it takes two for that tango. The example “Long Covid” subject is running at 1/5 of normal lung function (Fig. E3, below).
Lack of blood-flow (perfusion, or Q, in red) can have multiple causes. The best bet in the context of SARS-CoV-2 is spike-induced clotting and microclotting.
Lack of air-flow (ventilation, or V, in blue), outside of physical trauma, would typically suggest fibrosis or active inflammatory action (as I understand; pathology is my weak point). The authors did not find either. They did not perform additional tests that could shed light on the etiology for the widespread loss of ventilation function observed.
Typically, these types of scans seek to describe whether the problem is with getting air into the alveoli or getting blood into capillaries; in this case the V/Q mismatch paradigm isn’t helpful since so many subjects are experiencing both problems, either in different regions or in the same.
*edit, November 3: V/Q Mismatch, in terms of perfusion to un-ventilated regions, also explains deficiencies in oxygen saturation, as pulmonary flow to hypoxic (low oxygen) areas results in diluting the oxygen content of blood pumped to the rest of the body. The “match” of blood and air flow that keeps oxygen saturation near 100% is maintained by the Hypoxic Pulmonary Vasoconstriction reflex; which is further discussed here:
The Results
As children develop a robust, cross-reactive, and sustained immune response after SARS-CoV-2 infection41, the observed pulmonary dysfunction in our study is an unexpected finding.
To the authors’ surprise, only 1 of the infected kids showed a morphological anomaly.
Also to their surprise, below-normal lung function (airflow and bloodflow) was rampant — less than a third in either the “Recovered” or “Long Covid” groups had normal results.
The healthy controls:
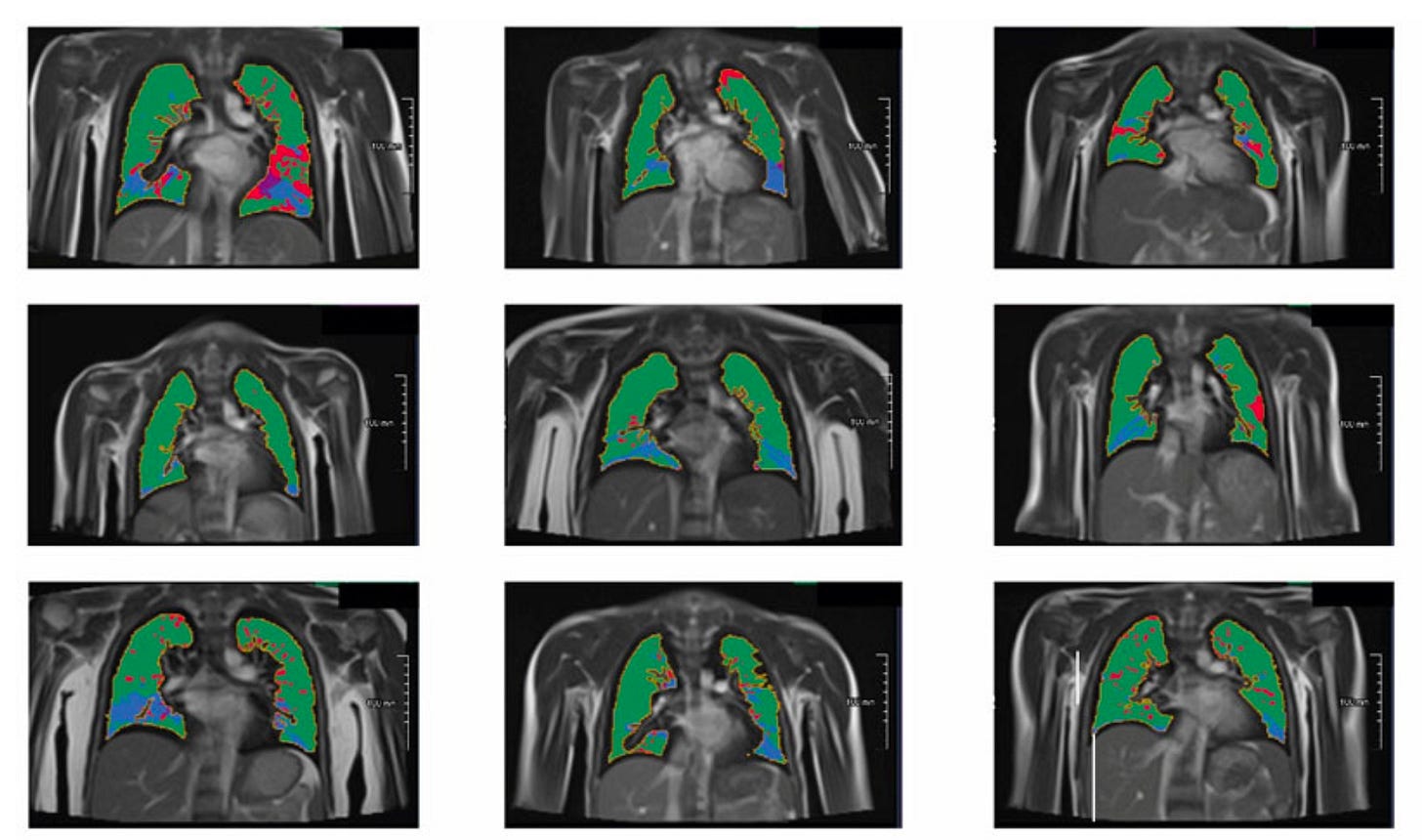
The “Recovered” group:
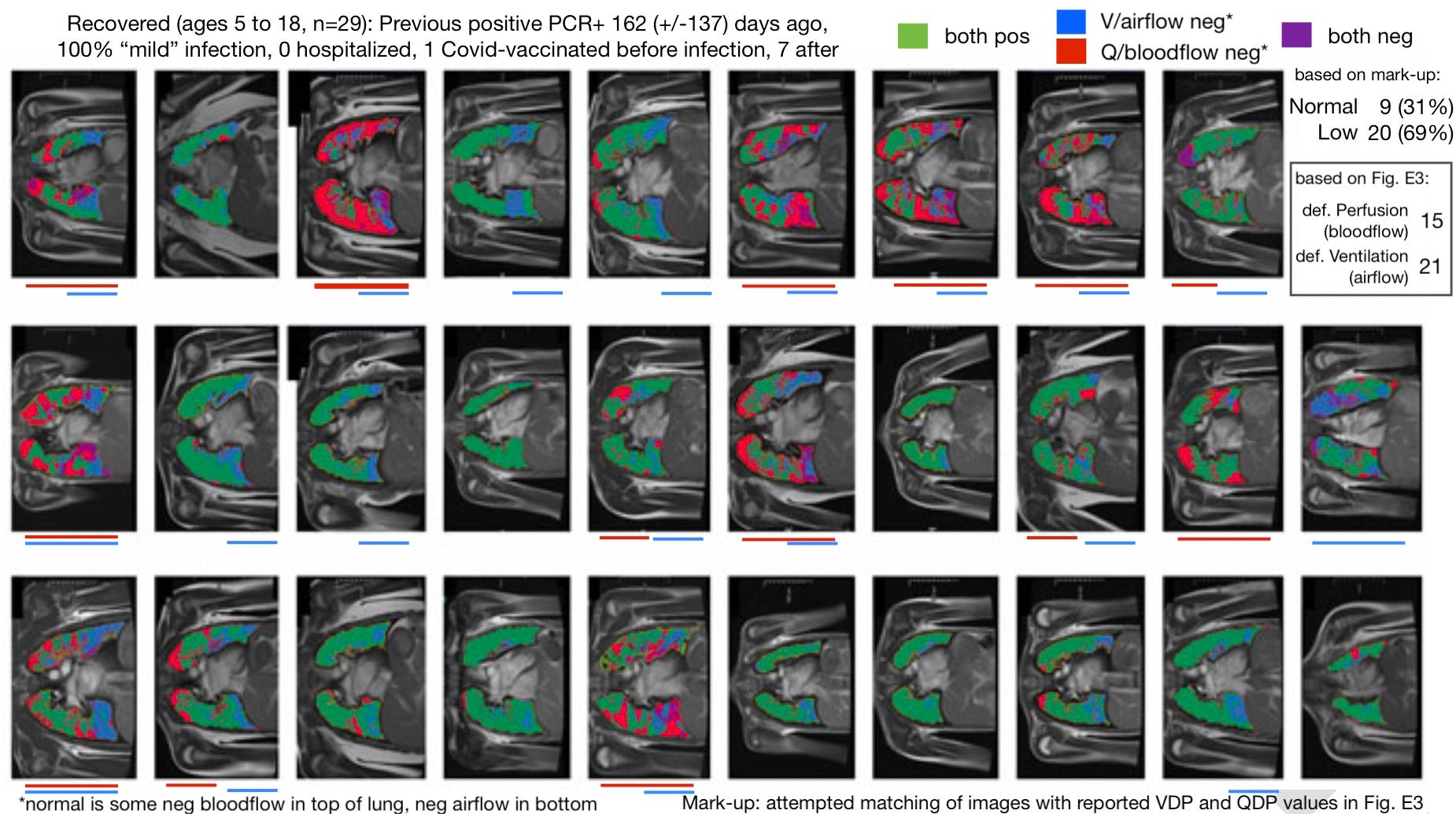
At first glance, it might seem like the big story here is the obstruction of blood-flow (again presumably due to micro-clotting). My markup of “low-airflow” subjects (blue bars) was influenced by the computer-generated results in figure E3 (below); only 8 of 29 “Recovered” score below 20% for defective airflow tissue (blue or purple), compared to 9 of 9 controls. So although it is hard to pick up the change by eye (in the end I could only figure out 19 of the 21 above-20%-ers), SARS-CoV-2 has apparently reduced airflow in over two thirds of recovered kids.
Post-SARS-CoV-2 infection in kids (“mild” infections, 0 hospitalized):
Reduced air-flow:
72% of “Recovered.”
Range air-flow reduced: 1 to 20%
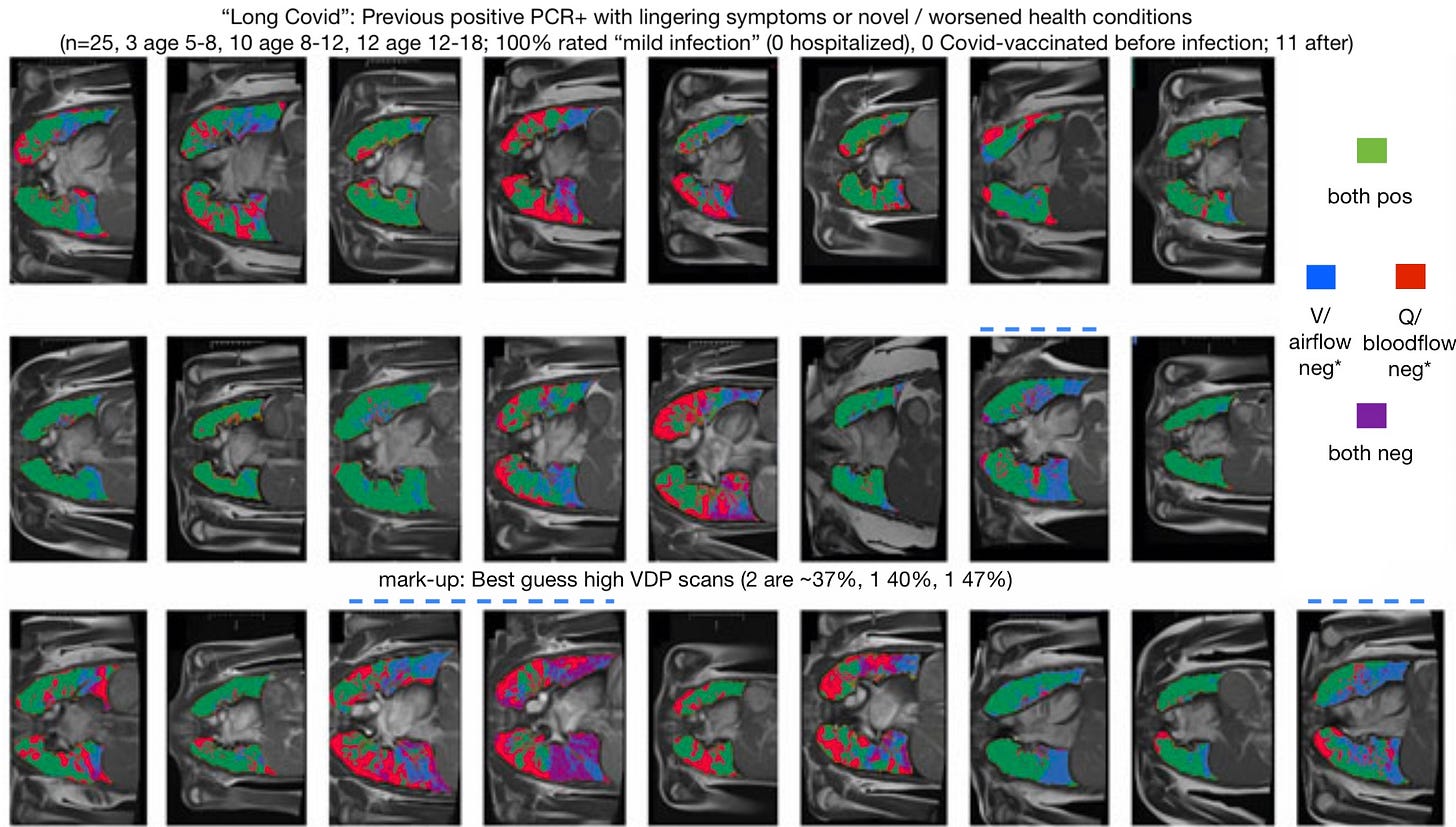
68% of “Long Covid.”
Range air-flow reduced: 1 to 28%
Reduced blood-flow:
52% of “Recovered”
Range blood-flow reduced: 3 to 55%
64% of “Long Covid.”
Range blood-flow reduced: 1 to 54%
Taking the healthy controls as a stand-in for the (unmeasured) pre-infection performance of the infected kids, mild SARS-CoV-2 infection seems to knock out airflow in up to a quarter and blood-flow in up to half of the lung. Reported long-term symptoms, incredibly, don’t seem to reflect this damage (except perhaps in that there are fewer “Long Covid” kids without reduced blood-flow).
And so, because the “Long Covid” group is overall not much different than the “Recovered” group, I did not repeat the same mark-up process here. Only the best-guess for the four outliers in airflow non-performance are highlighted:
Context: Nope, No Way This Is Normal
*edit, November 1, 2022: These results are potentially not as mysterious initially characterized below. Archer, et al. provide evidence for a means of facilitating blood flow to hypoxic (blue) areas (multiple coronavirus proteins impair the oxygen sensing function of arterial smooth muscle cell mitochondria, impairing Hypoxic Pulmonary Vasoconstriction in turn) and inaccessibility to air without fibrosis may simply be a result of lingering local pneumonia (fluid in alveoli). The HPV-impairment effect is also observed with normal human coronavirus proteins. One could further speculate that a demonstration of viral interference with the normal mechanism of restricting blood-flow to low-oxygen areas also suggests possible viral promotion of HPV. Mitochondria both inappropriately promote leaving open and closing local blood-flow in the lung.
Well, not really. But that is my first impression.
The SARS-CoV-2 panic has been fed in no small part by ignorance of the way the normal respiratory infection “sausage” gets made.
Viral qualities and infection outcomes that are in fact commonplace could be marketed as “novel,” due simply to the public’s unawareness of them.
This is still an important calibration to keep in mind with any new report regarding SARS-CoV-2 or the apparently magical spike protein which is just a bunch of amino acids, at the end of the day. The question must always be asked, “Compared to what?”
I feel the question can be skipped, here.
These kids’ lungs seem hugely clotted and mysteriously inaccessible to air. This is the most disturbing study on the virus I have ever seen. These are results I would expect in octogenarians, not children.
(But if I find a study on MRI scans after flu infections in children, I will post an update.)
Regarding healing.
I really don’t know what to think. If I was inclined to describe these as normal post-respiratory-infection changes, then it would be natural to predict eventual recovery. But I am not: These seem like aberrant results, either due to a property of the virus, or due to a hidden bias for extreme pulmonary involvement (as discussed below).
Dropping the Ball: No Comparison between injured and non-injured.
Heiss, et al. appears to have been designed with the intention of statistically demonstrating a marginal difference between the infected and control groups. For this reason, the authors prioritize grouping all the infected together and applying math to them as a whole.
This is nonsensical, as the infected are incredibly heterogeneous in lung non-function.
The burning question stops being, “Are the infected different than the controls?” but “What is different about infected who suffer lung dysfunction vs. those who do not?”
Is it age? Sex? Prevalence of certain symptoms during acute infection, including cough? Post-infection Covid-vaccination status? Such granular data could help distinguish between “kids and risk” vs. all kids.
Unfortunately, the raw data just isn’t there. The only granularity the authors provide is “time since positive PCR,” where they provocatively show that no kids more than a year from infection are at better than ~50% lung function (vs. the normal low 80%):

Off-hand, this strikes as a reflection of bias in both original testing (early tests in 2020 were typically in a clinical setting) and in still being interested in volunteering for the study.
Which brings us to:
It’s Got to Be Bias, Right?
The authors even acknowledge this possibility (if not likelihood):
Finally, a selection bias does exist, as families with children with acute or post-acute symptomatic COVID-19 and higher disease burden might have been more likely to participate in our study.
In other words, even though all these cases are reported as “mild,” they are still predominantly those that featured an aberrant level of lung involvement; even though fewer than half are reported as “Long Covid,” the others are still predominantly those in which a lingering lung injury is suspected by the parents.
If fewer than 1% of parents without any such suspicions replied to this trial’s recruitment pitch, compared to 100% who harbored the same suspicions, the observed rates of lung non-function would be completely unrepresentative of reality.
My tentative take on Heiss, et al. is that this must be the case.
Not because I am wedded to my many dismissals of the risk of the virus in children, or in humanity overall, but because I am 40 years old, and I would know if the virus had reduced my heart or lung function one iota. It seems preposterous that children could actually be faring so poorly: Wouldn’t we be seeing them hunched over, even fainting, all the time out in real life?
I haven’t observed any such evidence of disaster.
At the same time, Heiss, et al. is probably still showing something that is relevant to many children. It may be on the order of 1 in 100 or 1 in 1,000, rather than 1 in 2 as their results suggest: But it is still devastating.
If you derived value from this post, please drop a few coins in your fact-barista’s tip jar.
Heiss, R. et al. “Pulmonary Dysfunction after Pediatric COVID-19.” Radiology. 2022 Sep 20;221250.
“Long Covid” kids are more frequently post-infection injected, but don’t show much worse performance than the (already dismal) rates in the “Recovered” group.
However, it may turn out to be the case that the most long-ago infected are the most likely to be Covid-vaccinated; and these are disproportionately in the “Long Covid” group (based on the Elapsed time from positive RT_PCR in Table 2). It is thus possible that Covid-vaccination has aggravated rates of non-function in this set; but there is no way to parse this without the raw data.











Almost everyday, some new study. When will it be enough to convince you that you are under attack? We all are. Get with the program. Talking about it endlessly is waiting for them to ambush you. We need to get over it and face facts, we are under siege in a massive way. We can do something about it much better rather than wait till it slaps us in the face. We don't uphold proper principles like free speech and body autonomy. Nobody is calling for things like that that we can stand for. Everyone keeps saying the sky is falling. And it is but just repeating it over and over means it may fall on you. This is a time of great consciousness unfolding. You're either in it or you're bound for the train wreck.
I think this is a cohort issue. The groups in all 3 are very - very - small and one hence needs to wonder how they are selected. There are countless ways one can introduce bias. One thing that sticks out is 11 kids in group 2 were vaccinated AFTER having recovered from covid. That already suggest these are not randomly selected kids from all social groups.
I agree hence with the inherent selection bias conclusion. Group 2 is kids with symptoms afterwards. It is not 1000's of kids and see if they have symptoms, but recruiting the (extremely rare?) cases where there is a symptom. In other words, this may be data mining as opposed to sampling.
And last the control group was explicitly selected to NOT have any symptoms: "Healthy controls were excluded [...] current respiratory infection/symptomatology". If you take a random group of kids and see how many have a current respiratory infection/symptomatology, you have to exclude dozens of kids at any given time in a year. And especially in the study period August-December. It would be nice if they had taken a truly random sample and within that control looked for differences between those with and without any other respiratory infection/symptomatology.