The Swedish teen vaccine study, briefly
Results from a pre-print nationwide cohort study in Sweden are damning, but not in a way that exceeds what was already known.
A trio of researchers in Sweden do a science on the mRNA vaccines, comparing hospitalizations for Covid-19 or other causes in teens to estimate effectiveness and safety in the Omicron era.
Highlights:
Previous studies of Covid vaccine efficacy in youth were limited by being test-negative designs, or otherwise unreliable denominators. Hence the value of a nationwide comparison with a robust-sized unvaccinated group and little likely loss of follow-up.
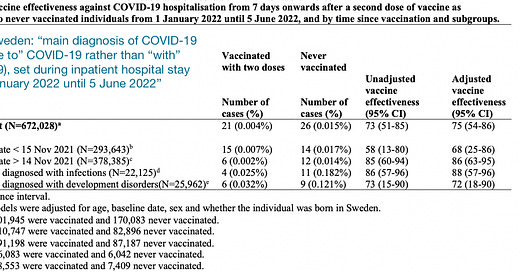
Apparent (double-injection) efficacy against Omicron hospitalization is 73%, which (after adjustment to 75% for demographics) translates to 11.4 prevented hospitalizations per 100,000 teens (my math), or a number needed to inject of 9,007 (the study’s math; 9,007 injected teens prevents 1 hospitalization; the other 9,006 get no measured benefit).
The safety analysis (based on any vs. no injections) claims to find no increase in hospitalization associated with the vaccines. This seems to be an effect of demographic disparities disguising obvious safety signals for myocarditis and a few other outcomes.
The study, posted online last week:1
Nationwide registers were used to examine the safety and effectiveness of COVID-19 mRNA vaccination against COVID-19 hospitalisation, and risk factors for COVID-19 hospitalisation in adolescents.
The safety analysis included all individuals in Sweden born between 2003-2009 (aged 11.3-19.2 years) given at least one dose of mRNA vaccine (N=645,355), and never vaccinated controls (N=199,022) [with follow-up start dates randomized to statistically resemble the first-injection mean and standard deviation dates]. Outcomes evaluated included all hospitalisations until 5 June 2022.
The vaccine effectiveness (VE) against COVID-19 hospitalisation and associated risk factors was evaluated in adolescents given two doses of mRNA vaccine (N=501,945), as compared to never vaccinated controls (N=170,083) [previously infected were excluded from both groups], during an omicron predominant period (1 January 2022 to 5 June 2022).
Findings 1: Efficacy
Regarding efficacy against hospitalization for Covid-19 during the Omicron period, it is reassuring that there were no signs of negative efficacy here (given, again, the limitations of previous studies that lacked reliable denominators).
Meanwhile, nothing is really impressive about positive efficacy given the rarity of hospitalization in teens during the study period. Only the “previous infections or developmental disorders” group had frequent enough Covid-19 hospitalization to result in a slightly less insane number-needed-to-treat value (1,031; estimated efficacy was the same in both groups, which is once again consistent with a “with, not for” effect). Meanwhile, the drop-off in efficacy for those reaching “dose 2 + 7 days” before mid-November is consistent with either genuine or “with, not for” efficacy:

The authors, whatever their priors, are thus on firm ground when offering the following conclusion, which despite the “may not” is strident compared to most vaccine double-speak:
Two doses were associated with a lower risk of COVID-19 hospitalisation during the omicron predominant period, especially among those with certain predisposing conditions who should be prioritized for vaccination. However, COVID-19 hospitalisation among general adolescents was extremely rare, and additional doses in this population may not be warranted at this stage.
Findings 2: Safety
The authors are less transparent when they report “COVID-19 mRNA vaccination was not associated with an increased risk of any serious adverse event in adolescents.” This is simply a reference to statistical tests failing to qualify any of the risk increases as “significant.” But a comparison of the rates reveals some clear red flags.
First, regarding overall hospitalization, it should be noted that the unvaccinated teens were less frequently native-born, which may translate to lower household income levels and higher background care levels (regardless of whether previous diagnoses reveal the same bias, since the same disparity may favor delays in care):

With that in mind, it is reasonable to expect that hospitalization rates should be lower in the vaccinated to begin with; with some cross-biases obviously confounding this expectation (for example, the disparity in prior diagnoses of anorexia in the vaccinated group is +.073% or 7 per every 10,000 teens).
With that in mind, the higher rates of certain diagnoses after the first dose in the vaccinated group seem clearly related to injection when compared to the rates after randomly time-matched unvaccinated:

My orange highlights show a clear trend for increased hospitalization codes for infection-related ailments, despite near-equal pre-follow-up rates in everything except for Mononucleosis. Meanwhile, red highlights the obvious culprits of myocarditis and pericarditis, as well as a stark reversal in the pre-follow-up balance for nephritis (kidney inflammation). Blue highlight is credited to efficacy against rare outcomes from hospitalization for infection with SARS-CoV-2.
It doesn’t look like a good trade-off. Given that virtually no teens are at risk from the virus, how could it ever have been one.
If you derived value from this post, please drop a few coins in your fact-barista’s tip jar.
Nordström, P. Ballin, M. Nordström, A. “Safety and effectiveness of COVID-19 mRNA vaccination and risk factors for hospitalisation caused by the omicron variant in 0.8 million adolescents: A nationwide cohort study in Sweden.” medrxiv.org






75% is a very high estimate. You’d really have to look at a different number: let’s say only 2 teens out of 100,000 would have needed hospitalization. Did the injection cause less hospitalizations in those 2 people? It’s impossible to say. When the risk is already so low for teens; it’s absolutely impossible to say that the vaccines dropped their risk. Yet we CAN say that the vaccines causes cardiac AES in a lot more than 2 people.
Brian, do you think that table 2 describes hospitalizations, as per last page of the study's flowchart?