Diphtheria: The Forgotten Mystery
Urbanization, and the "plague among children" that emerged from nothingness
Summary
Diphtheria, like polio, was once an almost-unknown disease in humans and children:
When he first entered on his duties (1858) “diphtheria had recently begun to be a source of much alarm to the public and great interest to the medical profession as a disease which (though it had been experienced in former times) was well-nigh unknown to the existing generation of British medical practitioners.”1
[P]revious to 1860 diphtheria was comparatively a rare disease in this country, so rare that in the report of the board of health of Philadelphia in 1859 no cases of diphtheria were reported2
-1891
In terms of its contribution to total mortality [in Sweden], diphtheria was nearly insignificant between 1775 and 1830. After 1860, the disease grew in importance, and in the 1880s accounted for as much as 5 per cent of all mortality in Sweden.3
-1994
In the late 19th century, the incidence of diphtheria radically increased, resulting in a curious paradox: While deaths from other infectious diseases began to decline, diphtheria deaths exploded throughout the West. Diphtheria quietly and curiously demanded a “last-minute” seat at the table of the scourges of childhood (such as measles and scarlet fever), despite widespread improvements in nutrition and sanitation in the mid and late century.
And, again like polio, the emergence of diphtheria epidemics created a specific, mostly-new type of disease.
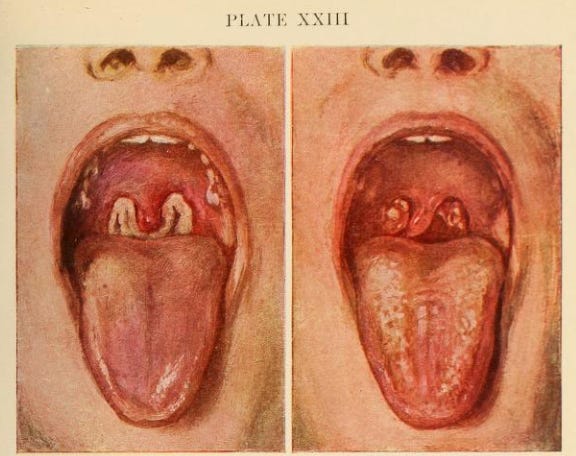
The bacteria responsible for clinical diphtheria produce a “toxin,” or more simply a “poison” — a molecular bioweapon which sabotages cellular protein synthesis, resulting in tissue death and organ damage. The toxin is found to be harmful to all manner of mammals, and domestic mammals as well perhaps as birds are also hosts which may briefly transmit toxin-producing diphtheria bacteria back to children.4 Infected children suffer from toxin distributed in the bloodstream and in the respiratory tract. Death is frequent in clinical cases of diphtheria — 29.7 to 42.4% of hospitalized cases were fatal in London, Boston, and New York in 1885-18945 — and preceded by the formation of a thick membrane of killed tissue in the upper respiratory tract, which “strangles” the patient from inside-out. Deaths of course also result from toxic paralysis of the heart and respiratory muscles.
It is this membrane which reliably marks a case of diphtheria, even if the same toxin can be produced by other types of bacteria harboring the same viral code, or if the toxin can manifest disease with other local and systemic effects.6
For such a distinctive and violent childhood illness to go from rarely-described to regular, demands explanation. Were it common, it could not have simply escaped notice before it was named, in 1826. Such a casual solution might seem to suffice if merely considering infant mortality as a statistic — a set of numbers within books resulting from poverty and thus neglect — but the absence of a disease such as diphtheria in more biographical accounts, describing the childhood of aristocrats and merchants, is glaring. There is not to my knowledge any equivalent in diphtheria to hold up to young Mozart’s bout with smallpox in 1767, for example. Therefore, diphtheria as a disease likely was rare, indeed unknown, before it was commonly observed.
This forgotten mystery — when and why did diphtheria emerge as a common cause of epidemics and death in childhood — ought to be a prime topic of modern research in human infectious disease. Instead, even though there is a field of research termed “emerging” diseases, the emergence of diphtheria is rarely questioned or even remembered as such — this is a bit absurd.

The case presented here will be that diphtheria epidemics were a late-onset outcome of urbanization. The timing of the transition to endemic-epidemic diphtheria (or endemic toxigenic diphtheria) was determined by relative transmission advantages between toxigenic and milder strains of the bacteria (Corynebacterium diphtheriae), with the milder strains having an initial advantage due to founder effects — inertia from rural dominance, essentially — which decayed over the course of the 19th century.
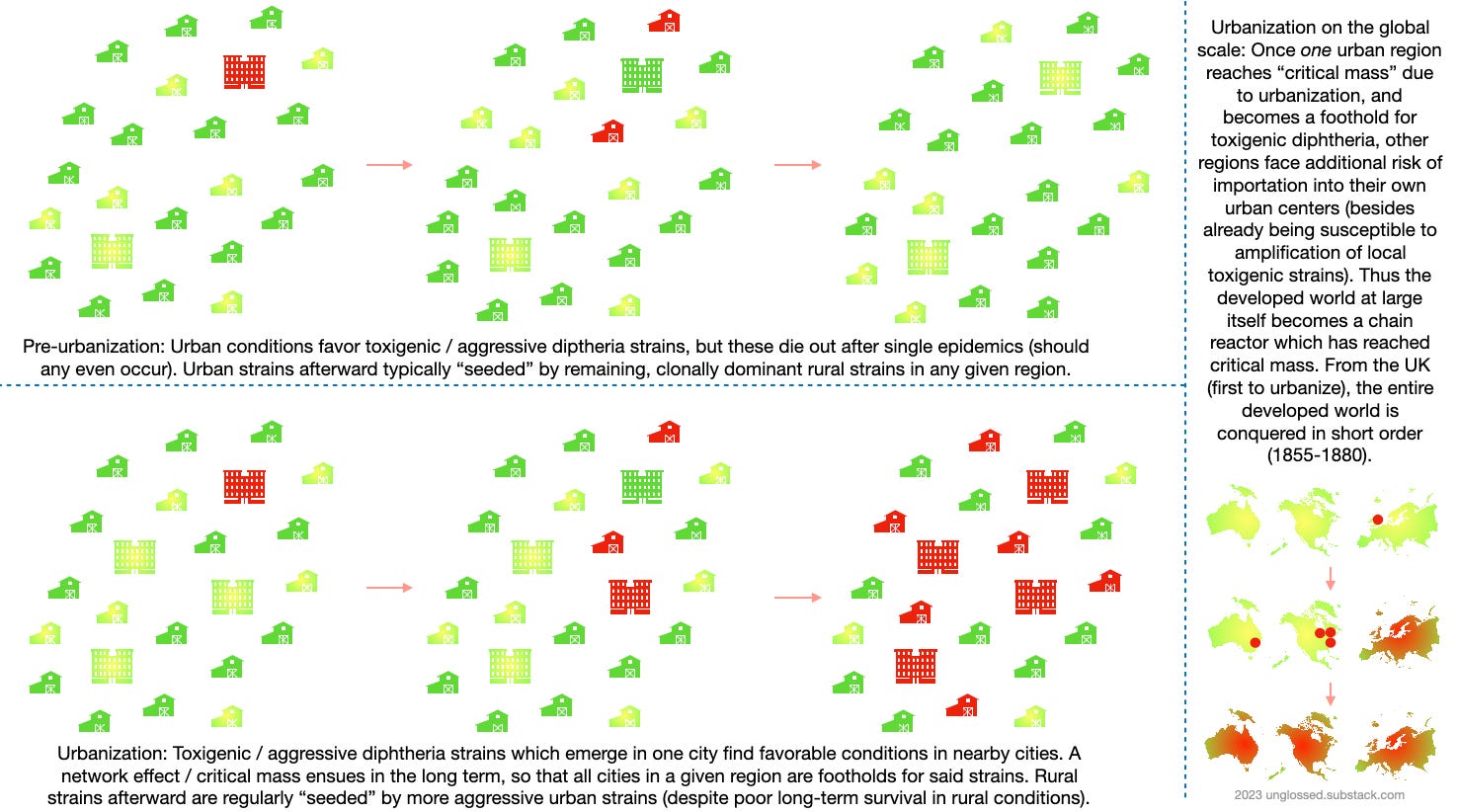
The wide-scale movement into cities in the 19th century created favorable conditions for the more aggressive and toxigenic strains of diphtheria, which previously would be limited by their tendency to sicken and kill their hosts. The expansion and founding of multiple large cities, in particular, created a network effect, wherein the growth in one city of toxigenic strains accelerated the growth of these strains in other nearby cities, and vice versa. Over time, the displacement of milder strains in most or all urban centers resulted in the “infestation” of the urban West, with toxigenic strains enjoying a permanent foothold in cities and spreading regularly into nearby rural areas from there.
The false memory of “eternal diphtheria”
This section may be skipped; it serves only to establish that there is a “default” understanding of diphtheria which includes substantial historical gaps.
In the course of my research on polio, I have come to notice a remarkable gulf between what is remembered about diphtheria in the West and what actually took place. This false memory obscures the story of how humanity spurred the emergence of, and eventually recovered from a horrible disease.
The typical account is along the lines of that given at History of Vaccines: Diphtheria was a scourge of childhood at the turn of the 20th century, with little cure before antitoxin (and no big deal is made of antitoxin), and finally, the vaccines came down from Heaven to save us. Antitoxin is mentioned, but no impact on the prevalence of disease is described, and the technology is portrayed as a fumbling precursor to later vaccines.
If a vaccine was not possible, perhaps an antitoxin might help?
This is a nonsensical portrayal of the topic. Antitoxin wasn’t known until it was developed for diphtheria in 1893. “Vaccines” barely existed outside of smallpox (which involves scraping pus into shoulders). And the modern science of immunology — resulting in Elrich’s Noble Prize in 1909 — was nursed with the study of antitoxins (i.e. antibodies), not human vaccines.
Setting aside for a moment the jumbled and misleading picture of antitoxin provided at History of Vaccines, a striking oddity appears in their description of the very beginning of the diphtheria story:
1613
Spanish Epidemic
This year was known in Spain as “El Año de los Garatillos” (“strangulations”) for its epidemic of diphtheria.
1735
The Plague Among Children
A terrifying diphtheria epidemic swept through New England. In some cases, entire families died of the disease. In one New Hampshire town, 32% of children under 10 died of diphtheria. The case-fatality ratio was almost 40%. Noah Webster (1758-1843) later wrote: “It was literally the plague among children. Many families lost three of four children—many lost all.” Treatments were largely ineffective.
1826
Diphtheria Given Its Name
Diphtheria, which had previously been called by a variety of names, gained its official name from French physician Pierre Bretonneau (1778-1862), who called the disease diphtérite.
And that is it — no description is provided for how diphtheria transitioned from a rare, localized “plague” without a name to a universal childhood disease causing, just for example, 86,138 deaths in Italy in the half-decade before 1893. Did this transition happen before or after it was named? It cannot be accepted that simply naming the disease explains this transformation. When and why does diphtheria become common?
The History of Vaccines account is more detailed, but otherwise substantially similar to the overview of the “prevaccine era” provided by Vitek and Wharton, in their paper discussing the post-Soviet epidemics in the early 1990s:7
In the prevaccine era, diphtheria was a dreaded, highly endemic childhood disease found in temperate climates. Despite a gradual decline in deaths in most industrialized countries in the early 20th century, which was associated with improved living standards, diphtheria remained one of the leading causes of childhood death until widespread vaccination was implemented. In England and Wales [which did not embrace diphtheria toxoid vaccination in 1926, unlike most of the West], as recently as 1937 to 1938, diphtheria was second only to pneumonia among all causes of childhood death, with an annual death rate of 32 per 100,000 in children less than 15 years of age.
This is a bit misleading, as rates of many individual diseases had only recently dropped to just below diphtheria. But again the obvious problem, the little puzzle in the history of diphtheria, becomes clear once they continue:
Superimposed on the high endemic disease rates was a rough periodicity of incidence with peaks every several years. Epidemic waves characterized by extremely high incidence and deaths were sporadic: Spain in the early 1600s, New England in the 1730s, and Western Europe from 1850 to 1890.
There is a glaring mystery here, but apparently one must resort to obscure sources to have it acknowledged. The diphtheria mystery isn’t part of the “groupthink” understanding of disease history, and so the incomplete history of the disease above is treated as sufficient, and diphtheria rarely comes up in discussions of “emerging” disease except in the context of the developing world in the late 20th century.
The mysterious emergence and paradox of diphtheria
In 1917, in his statistical survey of diphtheria, Crum offers the following history of the disease:8
Diphtheria as a cause of death was first so separately classified by the Registrar-General of England in 1855; it appeared for the first time in the New York City reports in 1857; and in the Massachusetts registration reports in 1858.
This seems… insufficiently curious. How is it diphtheria came to be so prevalent in the late 19th century? How common was it before it was “separately classified”? From Crum’s casual treatment of the topic, it is clear that the forgetting or obscuring of the novelty of diphtheria was already in place in 1917.
But more substantial acknowledgement of the novelty of diphtheria — not just as a “named” disease or reported statistic, but as a regular cause of epidemics — can still be found in 1889. A case report from this year gives the following background on the disease:9
When we consider the fact that previous to 1860 diphtheria was comparatively a rare disease in this country, so rare that in the report of the board of health of Philadelphia in 1859 no cases of diphtheria were reported, and [yet] in New York in 1883 there were 2090 deaths out of 3500 cases, over 59 per cent.; and when we see the literature of the day from all parts of the country treating of the ravages of this disease with its fearful rate of mortality, may it not be denominated the modern scourge?
Another acknowledgement of the novelty of diphtheria is provided by J Lewis Smith, writing in 1891:10
In New York city insanitary conditions and accumulations of refuse existed prior to 1850 even to a greater extent than at present, but without diphtheria. In the decade beginning with 1855 diphtheria was introduced, its germs, conveyed from the sick rooms by house drainage, entered the sewers, and now wherever the sewer gas escapes into the domiciles of this great city, it caries with it an outbreak of the disease. In all parts of the city children are constantly falling sick from inhaling the infected sewer gas, and it is chiefly from exposure to walking cases, and to sewer gas, that diphtheria is so prevalent in New York.
Both of these are still exceptions to the rule. Already in the 1880s, a sort of modified boiling-frog effect is in place in American newspaper reports. Inland regions with few cases of diphtheria and probable low reportage rates obsess over their own still-minor outbreaks, with demands for better control of the disease by local officials, to prevent a problem of the eastern coast from taking hold. These demands however fall amidst a backdrop of widespread lay indifference to the disease, until cases substantially increase. Thus in region after region, by the time the disease is common, attention is already focused on mitigation rather than explanation. Almost no one asks, “why this, why us”? It may be that similar factors operated outside of the anglosphere, in continental Europe.
To visualize the timing and scale of diphtheria’s emergence in America (and to some extent Canada), I have compared newspaper.com search results for “diphtheria” with some other diseases that would have had fairly consistent terminology throughout the decades in question. All counts are normalized to the combined results for “river” and “weather” over the same timespan, to adjust for the overall increase in the archived material being searched. (In other words, this visualizes how many times these diseases are mentioned for every so many times “river” and “weather” are mentioned.) The units are arbitrary, where “1” is the baseline, normalized amount of results for “diphtheria” in 1850-59. In the insert are the raw values per annum.

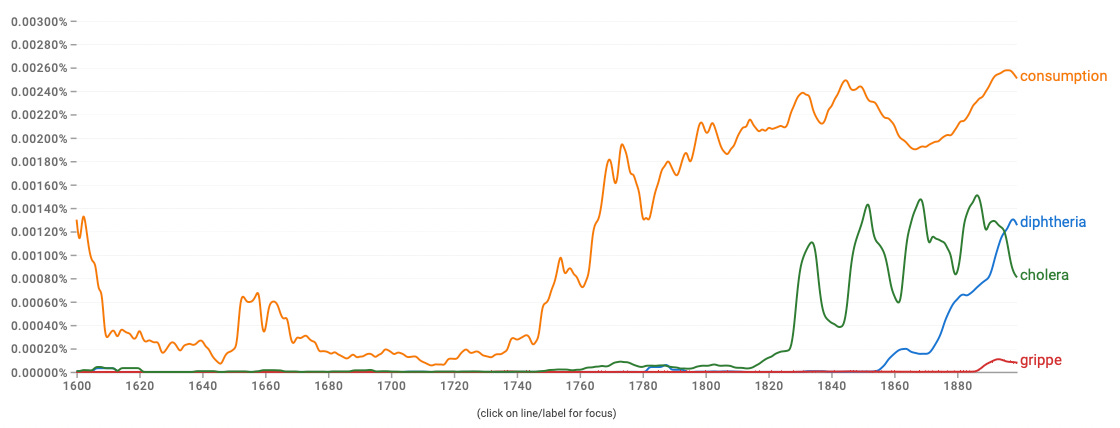
Consumption (tuberculosis) and cholera remain steady throughout the close of the century. “Grippe” increases dramatically with the epidemics of the 1890s. Amid this context, diphtheria emerges from being mentioned ~1/110th as often to ~1/3rd as often as cholera was in 1850. Results in Google ngram are not remarkably different:
A paradox in infectious disease
It is clear from both the above plots that diphtheria’s increase is belated compared to other infectious diseases exacerbated by urbanization.
Less clear is that it takes place when rates of death from those other diseases are declining, at least in adults. A narrative summary of the problem is that urban crowding and contaminated water brought forth the scourge of cholera in the early and mid 19th century; and eventually, the repeated occurrence of cholera epidemics resulted in state expansion and public health infrastructure; and yet for some reason, diphtheria epidemics emerge precisely when these same remedies begin to mitigate other causes of infectious mortality.
This results in the “diphtheria paradox” — even though cities begin to transition to publicly-regulated piped water and wastewater treatment after 1880, diphtheria becomes more and more widespread in the same era. Here it is appropriate to examine another graph from Nelson regarding Sweden, along with commentary:11
It is clear from the early studies of Rosén von Rosenstein and others that diphtheria did exist within the country, but was probably not widespread during the eighteenth century, with the exception of the period 1755-1761 when it was reported from several parts of the realm. The highest rates of diphtheria mortality in 1811-1830 were at most 12 deaths per 100,000 population. […] During the first two decades of elevated diphtheria mortality, deaths from the disease were as high as 84 per 100,000 in the countryside and even higher in the towns and cities.
The problem has now been depicted; the solution, though simple, asks for a bit more context on urbanization, sanitation, and diphtheria strains.
The solution
Context, 1: Urbanization
In most of the West, which is to say outside of England, urbanization is a phenomenon of the mid and late 19th Century.
A brief summary of values from Paul Bairoch and Gary Goertz suffice to tell the story:12 In 1700, London and Paris were the largest cities in Europe, the former counting 550,000 inhabitants. A century later, 23 of 211 million inhabitants of the future developed world lived in towns or cities, with an annual absolute growth rate of .1% of total population (270,000) over the next 30 years. In the period between 1830 and 1880, the annual growth rate was .5% (1,300,000); from 1880 to 1914 it was 1.1% (3,500,000). Urban growth in per-capita terms is slower between 1914 and 1950; and after 1950 takes on a different meaning due to suburbanization, with less relevance to overcrowding and disease. Thus, the era of rapidly increased urban crowding in the West primarily falls between 1830 -1914, with cities entering an era of desaturation and slum clearance afterward.
Cholera
If the beginning of the urbanization era is pinned to 1830, then cholera emerges almost instantaneously, with the first epidemics in 1831 (the United Kingdom) - 1833 (Portugal and Spain). Obviously, diphtheria — which emerges decades later — is a late-comer. But this does not mean it was not a result of urbanization; only that the effect was perhaps more delayed than for cholera.
Context, 2: Nutrition and Sanitation (vs. Overcrowding)
Nonetheless, Western mortality rates begin to decline in the earliest decades of the urbanization era, reach equilibrium in the early overcrowding era, and then decline again. This suggests two factors related to industrialization relieving mortality. Although the modern collective imagination tends to guess that medicine is responsible for these advances, no medical intervention besides smallpox vaccination credibly reduces mortality from diseases before the 20th century; and smallpox is never more than a minor contributor to deaths. And, as just reviewed, over-crowding in urban centers is not reduced until after 1914.
Therefore it is likely that improved nutrition and sanitation are the two factors responsible for reduced mortality rates in the latter half of the 19th century. To give an idea of the relative contribution of each, here is reproduced the model created by Thomas McKeown in 1965.13 The solid lines after 1838 are produced from British public records. The dashed lines in the era beforehand represent McKeown’s own assumptions:
Not reflected in the above graph is a reduction in deaths from tuberculosis starting in the 1850s. The timing of this reduction leads to the following conclusion:
The evidence in respect of diet is highly suggestive. The increase in tuberculosis mortality in both world wars is most plausibly attirbuted to a deterioration of nutrition. And in the 19th century, the time at which we can be fairly confident that mortality began to decline rapidly — the fifth decade — is also the time we can be reasonably certain that the standard of living began to improve. But although a better diet is not the only consequence of a higher standard of living, it is probably the one which is relevant in this context, as there was no significant reduction in crowding at home or at work. We conclude that improvement in diet was probably the main decline of mortality from tuberculosis during the 19th century.
This crude excerpt of McKeown’s work is provided merely to give the reader a general idea that nutrition likely improved concurrent to urbanization, mitigating the ill-health effects of crowding which did not find any direct relief until the next century.
However, the statistically recorded overall decline in mortality in England and Wales begins in 1870, and therefore seems primarily driven by improvements in sanitation and water quality. This follows two decades of expanded urban water supply coverage and reduced share of private companies in the same markets.14
The construction of the new sanitation system of London began after the great stink of 1858. Along with the construction of the new sewerage system in London, there were some developments in other cities of the United Kingdom. The rapid increase in water supply coverage of large cities that had initiated between the 1830s and the 1850s continued until the early 1870s. The percentage of large cities studied by Hassan (1985) that were supplied with piped water rose from 74 % to 96.3 % between 1851 and 1871. So it can be stated that the most important cities of the UK were supplied with piped water at the beginning of the 1870s. However, while the increase between 1830 and 1850 was accompanied by a rise in the share of private companies, between 1851 and 1871 the share of public companies in large cities rose from 26.5 % to 57.7 %. The transition from private to public control of water supply was accompanied by an increase in output and quality service. Average consumption increased 579 % in Manchester between 1841 and 1875, 153 % in Leeds between 1851 and 1871, and 66 % in Glasgow between 1845 and 1871. This was a result of the sales-maximizing goal of public companies that replaced the profits-maximizing goal of private companies.
After 1870, improvements in sanitation and water supply take hold throughout the urban West, though working-class districts and overcrowded slums are frequently the last to modernize.
In general, it can be said that the emergence of diphtheria epidemics does not seem explained by poor nutrition or unsanitary conditions. Both of these problems were ameliorated in absolute and per-capita terms in the late 19th century.
Therefore — if urbanization was the culprit explaining diphtheria — the feature of urbanization which was last to be relieved, overcrowding, is more likely to have been influential in the emergence of epidemics.
Context, 3: Diphtheria strains
Diphtheria has milder and more virulent strains. There are four primary types of diphtheria bacteria, with varying degrees of observed virulence — but all may express diphtheria toxin.
Measured in terms of case fatality, the most pathogenic strains of diphtheria are not always so obviously more severe than other strains. However, reliable measurements of mild and asymptomatic infection with different strains has always been nearly impossible. Small differences in apparent case fatality rates may reflect extreme differences in infection fatality rates. At all events, exposure to any strain of diphtheria may result in an asymptomatic infection that, over the long term, still trains the immune system to develop antibodies that protect from “toxigenic” strains (due to a slower or more gradual dosage of toxin). Assuming that toxigenic diphtheria did not evolve out of nowhere in 1855, it is likely that the absence of disease reflected “natural immunization” from frequent exposure to less pathogenic strains (and more gradual toxin release) in childhood. More pathogenic strains, before 1855, were simply rare.
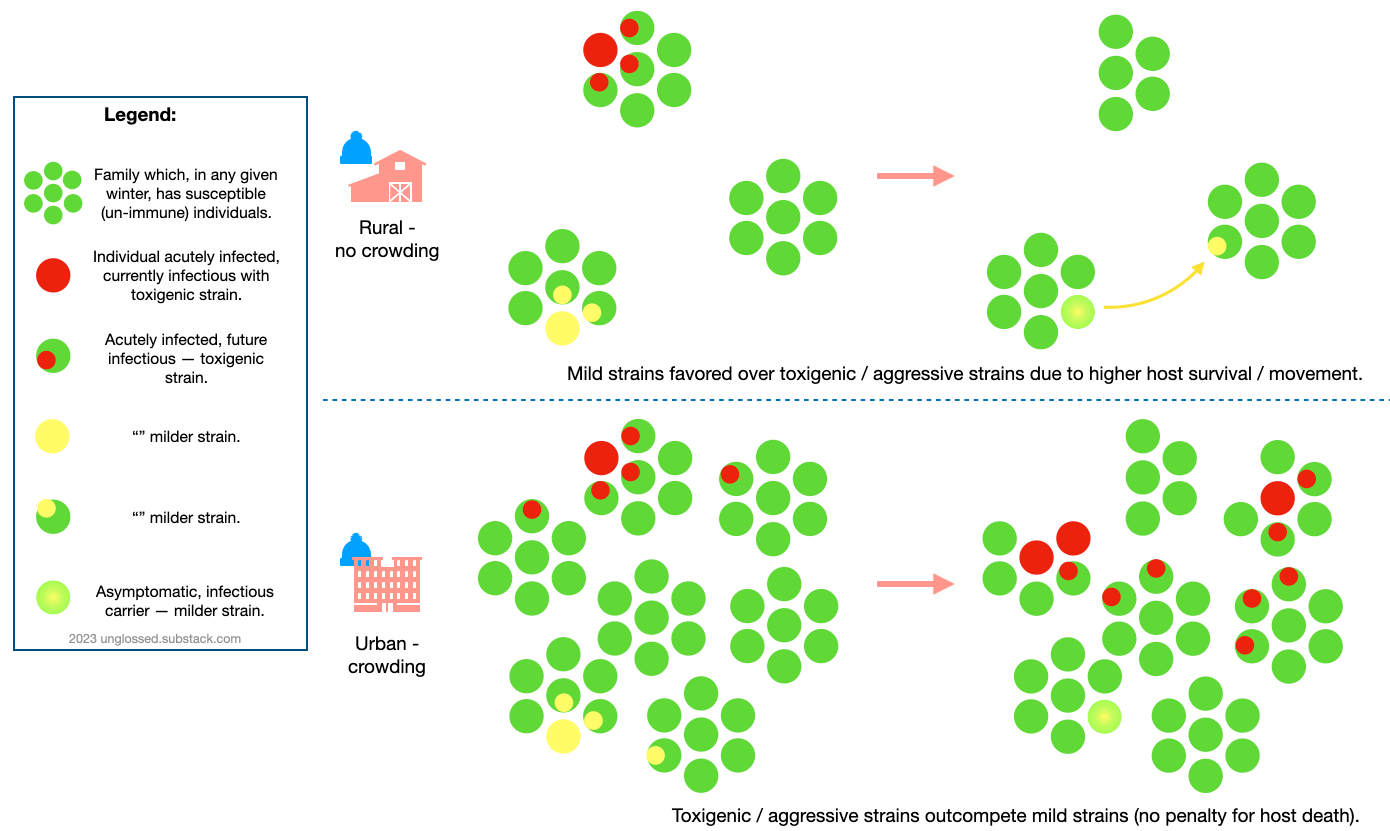
Whatever determines the virulence of given diphtheria strains — presence of the prophage genes encoding toxin, or intrinsic aggressiveness, etc. — diphtheria bacteria likely adhere to the trope that less pathogenic strains have an intrinsic transmission advantage, at least when transmission depends on keeping the host alive.
More toxigenic or aggressive strains, by causing increased rates of sickness and death, were kept rare before 1855 due to limited transmission.
Urban crowding, by regularly providing opportunities for early (prodromal) diphtheria secondary infection, removed the fitness penalty that previously kept more toxigenic / aggressive diphtheria strains in check. Instead, the rule in this new fitness landscape was “move fast and break things.”
Conclusion
Thus, urbanization introduced conditions favorable to widespread dissemination of more pathogenic diphtheria strains, the same way later developments (injections, etc.) created favorable conditions for HIV. In both cases, some decades passed before the pathogens in question reached a “critical mass” in one region — but once they did, global spread was almost instantaneous.
The following figures represent crude models of the dynamics just described. First, is shown the somewhat cliche notion of the fitness advantage afforded to less pathogenic strains of microbes. While I have reservations over this cliche when it comes to some viruses, I think it is an appropriate model for a ubiquitous commensal bacteria like diphtheria:
The next model portrays a similar dynamic resulting from the proliferation of cities within a region — just as individuals within a city are more likely to sustain chains of transmission of virulent strains (instead of the same strains dying out), regions with many cities are more likely to foster a “chain reaction” due to network effects, resulting in the same strains gaining a permanent foothold locally.
Alternate explanations
Alternate explanations are either the “institutionalization” of children in the form of orphan asylums and public schooling, or changes in livestock and products derived from livestock.
Though in a sense these changes are better timed to match the emergence of diphtheria epidemics after 1880, I find them implausible. These will be elaborated in a follow-up to this post.
If you derived value from this post, please drop a few coins in your fact-barista’s tip jar.
Gale, AH. (1945.) “A century of changes in the mortality and incidence of the principal infections of childhood.” Arch Dis Child. 1945 Mar;20(101):2-21. doi: 10.1136/adc.20.101.2.
J Lewis Smith. “About Diphtheria.” Syndicated in Lancaster New Era. September 12, 1891. p 2. newspapers.com
Marie C. Nelson (1994). “Diphtheria in late-nineteenth-century Sweden: policy and practice.” Continuity and Change, Volume 9, pp 213-242 doi:10.1017/S0268416000002277
It is unclear if diphtheria toxin toxicity has been investigated outside of mammals. My instinct is that the toxin does not depend on receptors specific to any phylum of animal, even if the bacteria usually endemic in humans is more discriminating. Early remarks on diphtheria mention that birds seem capable of spreading the disease to humans.
e.g. “Safety from Diphtheria.” The Times-Picayune. January 14, 1889. p 2. newspapers.com
From England also comes the report of an instance where diphtheria was carried by a turkey. A fowl with diphtheria was brought to a house of a veterinary surgeon and died five days later. The feeding and nursing of this bird devolved upon a lad aged 14, who was assisted by his baby brother, aged 5. In a little over a week after the death of the turkey the smallest child was taken ill with diphtheria, and the disease appeared in his brother next day, and about that time a sister of 9 years was also attacked. […]
The sudden appearance of this disease on [Skiathos in 1887] was quite a surprise to Dr. Paullinis, who had not seen a single case of diphtheria during thirty years. After a careful investigation of its origin he discovered that some days previously to the death of the first child a peasant living in the neighborhood of the house had received from Salonica a dozen pigeons. Two were very sick during the voyage and died of diphtheria as soon as they reached the island. [etc…]
Crum, FS. “A Statistical Study of Diphtheria.” Am J Public Health (N Y). 1917 May; 7(5): 445–477.
As always the correct term for viruses of bacteria are “phages,” but they are just viruses. Dormant phages integrate their genomes within bacterial chromosomes and often confer phenotypic traits, including synthesis of various proteins.
Vitek, CR. Wharton, M. “Diphtheria in the former Soviet Union: reemergence of a pandemic disease.” Emerg Infect Dis. 1998 Oct-Dec;4(4):539-50.
(Crum, FS. 1917.)
Coleman, PC. “Diphtheria; with Report of a Case Followed by Paralysis.” Daniels Tex Med J. 1889 Sep; 5(3): 81–83.
So the reader is not confused: Paralysis was a common complication of severe cases of diphtheria. It was typically short-lived and did not share clinical characteristics which define polio paralysis. There is no great likelihood that diphtheria paralysis contributed in any way to the earliest observations of polio epidemics.
(J Lewis Smith, 1891.)
(Marie C. Nelson, 1994.)
Bairoch, P. Goertz, G. “Factors of Urbanisation in the Nineteenth Century Developed Countries: A Descriptive and Econometric Analysis.” Urban Studies, Vol. 23, No. 4 (August 1986), pp. 285-305 (21 pages)
McKeown, T. “Medicine and world population.” J Chronic Dis. 1965 Nov;18(11):1067-77. doi: 10.1016/0021-9681(65)90002-0.
Abellán, J. “Water supply and sanitation services in modern Europe: developments in 19th-20th centuries.” Conference: 12th International Congress of the Spanish Association of Economic HistoryAt: University of Salamanca









On a kind of related topic, I came across these two papers recently which essentially explain why the modRNA vaccines cannot prevent the spread of the SARS-CoV-2 virus (note, I am not saying anything about whether they affect severity of the disease.)
Rethinking next-generation vaccines for coronaviruses, influenzaviruses, and other respiratory viruses
https://www.cell.com/cell-host-microbe/fulltext/S1931-3128(22)00572-8
Authors include Fauci and it is from 2022/2023.
"In this review, we examine challenges that have impeded development of effective mucosal respiratory vaccines, emphasizing that all of these viruses replicate extremely rapidly in the surface epithelium and are quickly transmitted to other hosts, within a narrow window of time before adaptive immune responses are fully marshaled."
SARS-CoV-2 replication in airway epithelia requires motile cilia and microvillar reprogramming
https://www.cell.com/cell/fulltext/S0092-8674(22)01505-7
Published a little before the one above. Authors from Standford.
This article provides exquisite descriptions of the mechanisms of entry and exit for various respiratory viruses and seems above reproach.
PAK1 blockers would seem to be useful, and D3 and IVM are PAK1 blockers but you can search for articles on those.
I had never heard of diphtheria until moving to the US, but then I lived in fairly spread out areas in Australia for my first 19 years. That is none of them had large populations. Also, there seemed to be no knowledge about it.
However, I just asked a person from Hong Kong if they had heard of it (or the Chinese name for it) and she had not. Also, a quick search revealed no info on the history of diphtheria in China, which is strange because they have had very large cities for quite a while and HK has been a large city for quite some time. Maybe opium was a bigger problem for them.